Introduction
Ankylosing spondylitis (AS) is a form of arthritis that causes major problems in the back due to inflammation of the spine. This inflammation leads to stiffness and pain in the back, chest and neck, significantly impacting daily life. It often begins in the late teens or early 20s, with symptoms progressive over time.
The persistent inflammation of ankylosing spondylitis leads to excess calcium production around the bones of the spine, called ossification. This can cause extra pieces of bone to form, contributing to back stiffness. Sufferers may experience severe stiffness in the morning, which decreases throughout the day with activity.
In severe cases, calcium buildup can cause some bones in the spine to fuse together, called ankylosis, accelerating curvature of the spine and limiting mobility. Besides stiffness and pain, chronic fatigue, poor appetite, and weight loss may also be present.
Ankylosing spondylitis is sometimes called Bechterew’s disease or Marie-Strümpell’s disease after the doctors who described it. Although the exact cause is not completely understood, genetic factors appear to play a role.
Diagnosis is based on a physical examination, medical history, blood tests and imaging studies. Early diagnosis is crucial for effective management, including anti-inflammatory medications, disease-modulating agents, and physiotherapy to maintain muscle flexibility and strength.
Epidemiology of Ankylosing Spondylitis
It is also important to note that ankylosing spondylitis tends to be more common in men than women, with a male-to-female ratio of approximately 2:1. It also has a higher prevalence in people with a family history of the disease, suggesting a genetic component.
According to available data, the incidence of ankylosing spondylitis is generally estimated between 0.1 and 2 cases per 1,000 people per year. However, these figures may vary depending on the populations studied and the diagnostic criteria used. Certain population groups, such as young men, appear to be at increased risk of developing ankylosing spondylitis.
These estimates may change over time as new epidemiological studies are conducted and awareness and understanding of the disease improves. It is always recommended to consult up-to-date medical sources and local epidemiological studies for the most recent data on the incidence of ankylosing spondylitis.
Ankylosing Spondylitis: Identifying the Causes
The exact cause of ankylosing spondylitis (AS) is not completely understood, but several factors may contribute to its development. Key considerations include:
- Genetic factors: AS has a strong genetic component. The presence of the human leukocyte antigen HLA-B27 is strongly associated with the disease. However, having this genetic marker does not guarantee the development of AS, and some people with the disease do not carry the HLA-B27 gene.
- Environmental factors: Although genes play a major role, environmental factors can trigger AS in genetically predisposed individuals. Infections, particularly those caused by certain bacteria, have been suggested as potential triggers.
- Autoimmune response: AS is considered an autoimmune disease. The immune system mistakenly attacks the body’s own cells, causing chronic inflammation of the joints and surrounding tissues.
- Heredity: Having family members with AS increases the risk of developing the disease. However, heredity alone is not enough to explain all cases.
- Sex and age: Men have a higher risk of developing AS than women. The disease often tends to manifest in individuals in their late teens or early twenties.
Although these factors are associated with AS, it is important to note that the disease can be complex and understanding its exact mechanisms still requires extensive research.
Understanding the Autoimmune Response in Ankylosing Spondylitis
Ankylosing spondylitis is in fact classified as an autoimmune disease. In this type of disease, the immune system, which is normally responsible for protecting the body against infections and pathogens, begins to mistakenly attack its own cells.
In ankylosing spondylitis, the immune system mistakenly targets cells in the joints and surrounding tissues, triggering chronic inflammation. This persistent inflammation leads to stiffness, pain, and eventually fusion of the spinal joints.
Although the exact cause of this autoimmune reaction is not fully understood, genetic factors appear to play a key role. Certain immune-related genes are associated with an increased risk of developing ankylosing spondylitis, suggesting a genetic predisposition to the disease.
Recognition of ankylosing spondylitis as an autoimmune disease directs treatment approaches toward modulation of the immune system. Medications used in the treatment of this condition often aim to suppress excessive immune activity, thereby reducing inflammation and alleviating associated symptoms.
Understanding that ankylosing spondylitis has an autoimmune component allows healthcare professionals to choose targeted therapeutic approaches to moderate the immune response and improve the quality of life of those affected by this disease.
Symptoms of ankylosing spondylitis
Symptoms of ankylosing spondylitis (AS) can vary from person to person, but they generally include:
- Back pain and stiffness: Pain and stiffness in the lower back are characteristic symptoms of ankylosing spondylitis. The pain may be intermittent or constant and worse at night.
- Morning stiffness: People with AS may experience significant morning stiffness, which can make it difficult to move when waking up.
- Fatigue: Fatigue is common in people with inflammatory diseases, including ankylosing spondylitis.
- Limitation of mobility: Due to joint inflammation, mobility of the spine may be limited. This can lead to a hunched posture.
- Joint pain and swelling: Besides the spine, ankylosing spondylitis can affect other joints, such as the hips, shoulders, knees, and feet, causing pain and swelling.
- Tendonitis: Some individuals can develop tendinitis, particularly in the heel (enthesitis).
- Eye problems: In some cases, eye problems such as uveitis may occur.
- Weight loss: Unintentional weight loss may occur due to illness and associated fatigue
It is important to note that these symptoms may change over time, and the severity may vary from person to person.
Pathophysiology of Ankylosing Spondylitis
Genetic Factors: Genetics play an essential role in predisposition to AS. More than 90% of people with AS are positive for the human leukocyte antigen HLA-B27. The presence of this gene is strongly associated with disease, although its precise relationship is not fully understood.
Inappropriate Immune Response: In AS, the immune system inappropriately attacks certain parts of the body, particularly the sacroiliac joints and the spine. This autoimmune reaction causes persistent inflammation.
Synovitis and Cartilage Destruction: The disease process underlying AS includes synovitis, an inflammation of the synovial membrane that lines the joints. This inflammation can lead to progressive destruction of articular cartilage.
Calcification of Ligaments and Tendons: Over time, AS causes calcification of the ligaments and tendons around the affected joints. This contributes to joint stiffening and loss of mobility.
Inflammation of Fibro-Osseous Junctions: Fibro-osseous junctions, particularly the intervertebral discs, also undergo inflammation. This can lead to symptoms such as stiffness and pain in the back, rib cage and neck.
Spinal Presentation of Ankylosing Spondylitis

Description:
Vertebral End Plates:Initial Ossification: Early signs of ossification with developing syndesmophytes along the edges of the vertebrae.
Partial Fusion: The vertebral end plates are beginning to show signs of fusion but remain distinct, indicating early stages of ankylosing spondylitis.
Stage: This is the early bamboo spine formation, where the spine starts to lose flexibility but has not yet reached full rigidity.

This image illustrates the progression of ankylosing spondylitis through four distinct stages. The first panel shows a normal spine, with well-defined vertebrae and clear intervertebral disc spaces, reflecting normal curvature and flexibility. In the second panel, inflammation is evident, characterized by soft tissue swelling and potential joint effusion, indicating early discomfort and stiffness, particularly in the sacroiliac joints. The third panel depicts the formation of syndesmophytes, where bony protrusions begin to develop along the vertebral end plates, with early calcification and ossification of the anterior longitudinal ligament. Finally, the fourth panel shows fusion, where the vertebrae are fully fused with the complete loss of intervertebral disc spaces, resulting in the characteristic “bamboo spine” appearance, with a rigid and straightened spinal column.
http://en.wikipedia.org/wiki/User:Senseiwa, CC BY-SA 3.0 <http://creativecommons.org/licenses/by-sa/3.0/>, via Wikimedia Commons
Understanding Entheses in Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a form of chronic inflammatory arthritis that primarily affects the sacroiliac joints (the joints between the sacrum and hip bone) and the spine. Entheses, which are the attachment points of tendons and ligaments to bones, are often the initial site of inflammation in AS.
When the immune system mistakenly attacks the entheses, it triggers an inflammatory response. This inflammation can cause symptoms such as pain, stiffness, and swelling in the affected entheses. Over time, persistent inflammation can lead to structural damage, such as fusion of the vertebrae in the spine, which can lead to loss of mobility.


Propagation of entheses
There are also two groups depending on the direction in which it spreads:
- Ascending variety: It starts from the sacroiliac joint and the lumbar vertebra and progresses towards the cranial parts, sometimes integrating the hips and knees.
- Descending variety: It starts from the cervical spine towards the caudal segments, it generally does not affect the large joints.

This image features a 6th-century skeleton with fused vertebrae, providing historical evidence of severe ankylosing spondylitis. The fusion of the vertebrae illustrates the advanced stage of the disease, characterized by the loss of spinal flexibility and the development of a “bamboo spine” appearance. This ancient specimen highlights how ankylosing spondylitis has affected humans across centuries, illustrating its long-standing impact on the human condition.
Attribution: Anagoria, CC BY 3.0, via Wikimedia Commons.
One Day in the Life of Someone Living with Ankylosing Spondylitis
Living with ankylosing spondylitis (AS) presents unique challenges, and each day requires careful management of symptoms to maintain a quality of life. Here’s a glimpse into a typical day for someone living with AS:
Morning Routine
The day often begins with stiffness and discomfort in the spine and joints, a common symptom of AS. Waking up can be difficult, and it may take some time to loosen up the body. Gentle stretching exercises, such as yoga or tai chi, are an essential part of the morning routine to improve flexibility and reduce stiffness. A warm shower can also help soothe sore muscles and joints, making movement easier.
Breakfast typically consists of anti-inflammatory foods, such as oatmeal topped with berries and nuts. Eating a balanced diet with anti-inflammatory foods helps manage inflammation and provides essential nutrients. Supplements like omega-3s, vitamin D, or turmeric may also be part of the morning regimen to further reduce inflammation and support joint health.
Work and Daily Activities
For many with AS, working in a traditional office setting can be challenging due to prolonged sitting and the need for ergonomic support. People often use standing desks or take regular breaks to stretch and walk around. Maintaining good posture is crucial, so ergonomic chairs and proper desk setups are essential. Some might use cushions or lumbar support to reduce strain on their backs.
If they work from home, they might incorporate short stretching sessions throughout the day to keep the spine mobile and prevent stiffness. Managing stress is another critical aspect of daily life, as stress can exacerbate symptoms. Practices like mindfulness, meditation, or deep-breathing exercises can be helpful in maintaining mental well-being.
Lunch includes nutrient-dense meals like grilled salmon with leafy greens and quinoa, which provide anti-inflammatory benefits and sustained energy.
Afternoon and Physical Activity
Regular physical activity is vital for managing AS symptoms. After work or during lunch breaks, a short walk or low-impact exercises such as swimming, cycling, or Pilates can help maintain joint flexibility and reduce pain. Physical therapy sessions might also be part of the routine to target specific areas of discomfort and strengthen supporting muscles.
Pain management is an ongoing consideration, and individuals might rely on prescribed medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or biologics, to control symptoms and prevent flare-ups. Over-the-counter pain relief creams or patches might also be used for localized relief.
Evening Relaxation
After a long day, unwinding is essential. Evenings are typically spent engaging in relaxing activities that minimize stress and promote overall well-being. This might include reading, watching a favorite show, or spending quality time with family and friends. Some people find relief in warm baths with Epsom salts, which can help ease muscle tension and pain.
Dinner might consist of anti-inflammatory dishes, such as a lentil and vegetable stew or grilled chicken with turmeric-spiced vegetables. Avoiding foods that can trigger inflammation, such as processed or sugary foods, is a key part of dietary management.
Before bed, gentle stretches or a session of guided meditation can help relax the mind and body, setting the stage for restful sleep. Maintaining a consistent sleep schedule is crucial, as poor sleep can worsen symptoms.
Sleep and Rest
Getting a good night’s sleep is vital for anyone with AS, as rest is essential for recovery and pain management. The night can be challenging, as some people may experience discomfort or wake up due to pain. Using supportive pillows and a firm mattress can aid in maintaining a comfortable sleeping position, reducing the risk of morning stiffness.
The Impact of Ankylosing Spondylitis on Spinal Mobility
As spondyloarthropathies, particularly ankylosing spondylitis, progress, complications such as syndesmophytes and ossification of the facet joints may occur, significantly impacting spinal mobility. These pathological manifestations play a key role in determining the long-term prognosis, closely linked to the limitation of the ability to move.
Syndesmophytes are bony growths that form along ligaments, often seen in the spine during ankylosing spondylitis. These growths can fuse the vertebrae together, leading to loss of flexibility and increased stiffness of the spine. This gradual fusion can cause the spine to appear stiff and straight, characteristic of the advanced stage of the disease.
At the same time, ossification of the facet joints, which are the small joints between the vertebrae, can also contribute to limited mobility. When these joints become calcified and stiff, spinal movement becomes increasingly restricted, impacting the ability to bend, turn, and perform normal daily activities.
The long-term prognosis of these spondyloarthropathies is closely correlated with the extent of mobility limitation. The more the fusion of the vertebrae progresses, the more the movements of the spine are compromised. This loss of mobility can lead to functional disability and limitations in daily activities, thus affecting the quality of life of affected individuals.
Management of these complications aims to alleviate pain, reduce inflammation, and, if possible, slow the progression of the spinal fusion. Medical approaches, such as the use of anti-inflammatory medications and biological therapies, may be considered. Physiotherapy and specific exercises aimed at maintaining mobility and preventing stiffness may also be included in the treatment plan.
In summary, syndesmophyte formation and ossification of facet joints in spondyloarthropathies can lead to significant loss of spinal mobility, directly influencing the long-term prognosis of these conditions. Early and careful management of these complications is essential to minimize their impact on the quality of life of affected individuals.
Assessing the Lumbar Spine in Ankylosing Spondylitis
Check for loss of lumbar lordosis using the Schober test
- The patient in a standing position
- To do this, we use two brands:
- L5 (approximately at the level of the posterior superior iliac spine) and 10 cm above the latter, in a standing patient.
- The patient is then asked to lean forward as much as possible and the increase in distance between the two marks made previously is then measured.
- The patient is asked to touch their toes with their knees extended.
- Normally, the two points should be more than 5 cm apart;
- If the lumbar excursion is less than 3 cm, it implies a loss of lumbar flexion suggestive of ankylosing spondylitis.

This image illustrates the Schober test, a tool used to evaluate lumbar flexibility and loss of lumbar lordosis. Two points are marked on the skin: the first at the L5 spinous level and the second 10 cm above it. During lumbar flexion, the distance between these points should increase to 13 to 15 cm. A reduction to 13 cm or less, or a noticeable decrease in lumbar lordosis, can indicate limited lumbar flexion and potential spinal abnormalities. The Schober test is valuable for assessing spinal flexibility and diagnosing conditions that affect spinal mobility, such as ankylosing spondylitis.
Risk factors
- Genetic predisposition:
- The strongest risk factor associated with ankylosing spondylitis is genetic predisposition.
- The presence of the genetic marker HLA-B27 is strongly linked to the disease. However, possession of this marker is not sufficient to guarantee the development of ankylosing spondylitis, and many people carrying HLA-B27 never develop the disease.
- Family history :
- Ankylosing spondylitis tends to occur more frequently in individuals with a family history of the disease.
- The genetic component may play a major role in the transmission of predisposition to ankylosing spondylitis.
- Sex and age:
- Men are more likely to develop ankylosing spondylitis than women.
- The disease often has an early onset, usually before the age of 40, although later cases can also occur.
- Infections:
- Some researchers suggest that bacterial infections, particularly gastrointestinal infections, may trigger ankylosing spondylitis in genetically predisposed individuals.
- However, the link between infections and disease onset remains an evolving area of research.
- Environmental factors :
- Environmental factors such as smoking have been linked to an increased risk of developing ankylosing spondylitis.
- Smoking is also linked to more severe disease progression.
- Other inflammatory diseases:
- The presence of other inflammatory diseases, such as psoriatic arthritis or inflammatory bowel disease, may increase the risk of developing ankylosing spondylitis.
Differential diagnosis
- Rheumatoid Arthritis (RA): Rheumatoid arthritis is an autoimmune disease that affects the joints. Although some similarities may exist with AS, rheumatoid arthritis tends to affect multiple joints, including the small joints of the hands and feet.
- Osteoarthritis: Osteoarthritis is a degenerative joint condition that occurs due to wear and tear of cartilage. It can cause similar symptoms to AS, but the location of the affected joints and the triggering factors may be different.
- Non-Radiographic Axial Spondyloarthritis (axSpA): This condition has symptoms similar to AS, but the radiographic signs are not yet visible. It can progress to ankylosing spondylitis over time.
- Common Low Back Pain: Lower back pain can be present in a variety of conditions, including common low back pain, which is not specifically related to inflammation of the sacroiliac joints.
- Systemic Lupus Erythematosus (SLE): Lupus is a systemic autoimmune disease that can affect various organs, including the joints. It may present with symptoms similar to AS.
- Crohn’s Disease and Ulcerative Colitis: These inflammatory bowel diseases can sometimes be associated with symptoms similar to those of AS, particularly regarding joint inflammation.
- Infections: Some infections, especially those affecting the joints, can cause inflammation and symptoms similar to those of AS.
Radiolgraphic signs
- Sacroiliitis – usually bilateral and symmetrical, affecting the lower third (synovium), particularly the iliac side of the joint. Loss of clarity of the joint edges, erosions, widening of the joint space with subsequent bony proliferation and sclerosis may be noted. As the changes progress, the boundaries of the joint space become increasingly blurred and gradually disappear as ankylosis develops.
- Spondylitis – erosions and new bone growth occur at the corners of the vertebral bodies, usually starting at the thoracolumbar junction, to form “Romanus lesions”. Bone then forms along the anterior surface of the vertebral body, reversing the normal concavity and creating a square appearance. Calcification develops in the neighboring intervertebral disc and longitudinal ligaments of the spine, forming syndesmophytes which can grow to form bone spurs and unite with similar lesions in adjacent vertebrae, resulting in a characteristic appearance of bamboo thorn and eventually causes ankylosis.
- Soft tissue calcification – ligamentous calcification may occur, for example in the posterior ligamentous portion of the sacroiliac joint. of the sacroiliac joint and the posterior interspinous ligament.
- Bone density – this may generally be reduced.
Sacroiliitis
Sacroiliitis is an inflammation of the sacroiliac joints, which are the joints between the sacrum (the triangular bone at the base of the spine) and the iliac bones of the pelvis. These joints are essential for spinal stability and are important for trunk movement, especially when walking.
Sacroiliac joint inflammation can be caused by a variety of medical conditions. Sacroiliitis is often associated with inflammatory diseases, particularly ankylosing spondylitis, which is a form of chronic inflammatory rheumatism primarily affecting the spine.
Symptoms of sacroiliitis typically include pain in the lower back, buttocks, and possibly the hip. This pain can be bilateral (affecting both sides) or unilateral. Stiffness and discomfort, especially after periods of inactivity, can also accompany sacroiliitis.
SI inflammation

The first symptom of ankylosing spondylitis is usually sacroiliitis, which is inflammation of the entheses of the sacroiliac joint. Inflammation of the sacroiliac joint can be secondary to osteoarthritis, pregnancy, spondyloarthropathy and trauma. Radiologically, sacroiliitis affects the synovial component of the sacroiliac joint, and the first observation is a decrease in the definition of the edges of the joint. Afterwards, the joint space becomes wider or irregular, and focal erosions develop, particularly on the iliac side of the joint, leading to sclerosis and ultimately fusion (ankylosis).
Fusion (ankylosis) SI

This image illustrates the fusion of the sacroiliac (SI) joint, a common feature in ankylosing spondylitis. The complete fusion of the SI joints is evident, showing the characteristic loss of joint space and formation of bony bridges.
Case courtesy of Assoc. Prof. Frank Gaillard,From the case rID: 35986
Spondylitis
Spondylitis is an inflammation of the vertebrae, characterized by an inflammatory condition in the spine. This inflammation can affect different parts of the spine, including the cervical, thoracic, lumbar vertebrae, or even the sacroiliac joints at the junction between the sacrum and the iliac bone of the pelvis.
Spondylitis is often associated with inflammatory diseases, and one of the best known forms is ankylosing spondylitis. The latter is a type of chronic inflammatory rheumatism that mainly affects the spine, causing inflammation of the sacroiliac joints and leading to the formation of syndesmophytes, bony growths.
Symptoms of spondylitis may include lower back pain, spinal stiffness, loss of mobility, persistent fatigue and, in the case of ankylosing spondylitis, a characteristic posture called “bamboo back” due to the fusion of the vertebrae.
Romanus lesion

This MRI radiograph displays a 35-year-old patient with inflammatory back pain, positive for HLA-B27 and uveitis. The image highlights a Romanus lesion, characterized by inflammatory changes at the vertebral end plates. The yellow arrow points to the “shiny corners,” indicative of bone marrow edema and erosion at the vertebral margins. These features are consistent with ankylosing spondylitis and illustrate the inflammatory processes affecting the spine.
Case courtesy of Prof. Craig Hacking, Radiopaedia.org. From case rID: 93780.
Romanus lesion (bright corners sign) is an early manifestation of ankylosing spondylitis and presents as an irregularity and erosion involving the anterior and posterior edges of the vertebral endplates. Repair of these inflammatory erosions appears radiographically as reactive sclerosis at the same location, known as the bright corner sign.
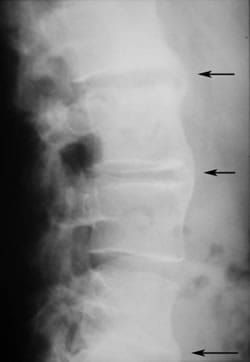
Squaring of the vertebral bodies

The lateral radiograph of the lumbar spine reveals characteristic changes associated with ankylosing spondylitis. The arrows highlight the squaring of the anterior aspects of the lumbar vertebral bodies, indicating the early formation of syndesmophytes. Additionally, ankylosis of the posterior elements is evident, showing fusion of the posterior spinal structures. These findings are indicative of progressive spinal rigidity and inflammation.
Ankylosing spondylitis is the most common cause of squaring (square appearance) of the vertebral body. It is associated with reactive sclerosis of the edges of the vertebral bodies (bright corner sign) typically in the lumbar spine. Squaring of the vertebral bodies occurs after the bright corner sign/Romanus lesion and precedes the bamboo column.
Marginal syndesmophyte

This image illustrates key radiographic features of ankylosing spondylitis. Fusion of the vertebral bodies due to marginal syndesmophytes creates the characteristic “bamboo spine” appearance. Ossification of the supraspinous and interspinous ligaments is evident, presenting the classic “Dagger sign.” Additionally, subchondral erosions, sclerosis, and proliferative changes are observed on the iliac side of the sacroiliac joints.
Case courtesy of Assoc. Prof. Craig Hacking, Radiopaedia.org.. From case rID: 93780
Represents the bony bridging connecting adjacent vertebral margins, which create the classic bamboo spine (vertebral ankylosis) in the advanced stage of the disease.
Bamboo-shaped spine

The bamboo-shaped vertebral column essentially results from the fusion of the vertebral bodies by marginal syndesmophytes. It may be accompanied by a fusion of the posterior vertebral elements. A bamboo-shaped spine typically presents at the thoracolumbar and/or lumbosacral junctions and perhaps prone to unstable vertebral fractures and Andersson lesions. In a bamboo-shaped spine, the outer fibers of the annulus fibrosus of the intervertebral discs ossify, resulting in the formation of marginal syndesmophytes between adjacent vertebral bodies. The resulting radiographic appearance is therefore that of thin, curved, radiopaque spicules that completely connect adjacent vertebral bodies. Together, these elements give an undulating appearance to the continuous lateral edges of the spine on AP radiographs of the spine and resemble a bamboo stalk, hence the term bamboo spine.

Soft tissue calcification
Dagger Sign
Single central radiodense line on frontal radiographs, associated with ossification of the supraspinous and interspinous ligaments secondary to enthesitis. It is possible that the radiodense line extends to the sacrum.

This image shows the “Dagger sign,” a classic radiographic feature of ankylosing spondylitis. The sign is characterized by the ossification of the supraspinous and interspinous ligaments, which appears as a radiopaque line resembling a dagger.
Case courtesy of Assoc. Prof. Frank Gaillard, Radiopaedia.org. From the case rID: 3382.
Differences between osteophytes and syndesmophytes
Osteophyte

Paravertebral ossification, horizontal orientation.
Claw Appearance
- Marginal: horizontal bony extension of the vertebral plate.
- Non-marginal: horizontal extension of the vertebral body 2-3 mm from the end plate.
Syndesmophyte

Paravertebral ossification, vertical orientation
Sharpey fibers arise which extend to the bone, and are therefore contiguous to the vertebral body.
- Marginal
- Originating at the edge of a vertebral body, extending to the edge of the adjacent vertebral body (ossification of the annulus fibrosus).
- Non-marginal
- Usually large and bulky
- Leave the vertebral body, away from the end plate or rim.
Recommendations
- Medical consultation :
- Consult a rheumatologist for an accurate diagnosis and a treatment plan tailored to your situation.
- Education about the disease:
- Learn about ankylosing spondylitis to understand its symptoms, progress, and treatment options. Reliable patient organizations and medical websites can provide valuable information.
- Medical treatment :
- Follow the treatment plan prescribed by your doctor, which may include anti-inflammatory medications, biological therapies, corticosteroids, and other medications depending on the severity of the condition.
- Osteopathy and Exercises:
- Physiotherapy can play a crucial role in maintaining mobility. Specific exercises and stretches may be recommended to strengthen muscles and improve flexibility.
- Pain Management:
- Learn pain management techniques which may include the use of heat, cold, or relaxation methods.
- Psychological support :
- Ankylosing spondylitis can have psychological impacts. Seek emotional support from mental health professionals, support groups, or loved ones.
- Lifestyle Adaptation:
- Make adjustments in your daily life to make the disease easier to manage. This may include workplace ergonomics, choosing an appropriate mattress, or adaptations in physical exercise.
- Regular Medical Follow-up:
- Schedule regular appointments with your rheumatologist to assess disease progression and adjust the treatment plan as needed.
- General Health:
- Maintain a healthy lifestyle in terms of a balanced diet, appropriate physical exercise, and stress management.
- Participation in Research:
- If possible, consider participating in ankylosing spondylitis research studies to help advance knowledge of the disease.
Extra-articular features of ankylosing spondylitis
- Anterior uveitis (25%) and conjunctivitis (20%)
- Prostatitis (80% of men): generally asymptomatic.
- Heart disease
- Aortic incompetence
- Mitral incompetence
- Cardiac conduction defects
- Pericarditis
- Amyloidosis
- Atypical fibrosis of the upper lobe of the lung
- Extra-articular features of ankylosing spondylitis
- Medical consultation :
- Consult a rheumatologist for an accurate diagnosis and a treatment plan tailored to your situation.
- Education about the disease:
- Learn about ankylosing spondylitis to understand its symptoms, progress, and treatment options. Reliable patient organizations and medical websites can provide valuable information.
- Medical treatment :
- Follow the treatment plan prescribed by your doctor, which may include anti-inflammatory medications, biological therapies, corticosteroids, and other medications depending on the severity of the condition.
- Physiotherapy and Exercises:
- Physiotherapy can play a crucial role in maintaining mobility. Specific exercises and stretches may be recommended to strengthen muscles and improve flexibility.
- Pain Management:
- Learn pain management techniques which may include the use of heat, cold, or relaxation methods.
- Psychological support :
- Ankylosing spondylitis can have psychological impacts. Seek emotional support from mental health professionals, support groups, or loved ones.
- Lifestyle Adaptation:
- Make adjustments in your daily life to make the disease easier to manage. This may include workplace ergonomics, choosing an appropriate mattress, or adaptations in physical exercise.
- Regular Medical Follow-up:
- Schedule regular appointments with your rheumatologist to assess disease progression and adjust the treatment plan as needed.
- General Health:
- Maintain a healthy lifestyle in terms of a balanced diet, appropriate physical exercise, and stress management.
- Participation in Research:
- If possible, consider participating in ankylosing spondylitis research studies to help advance knowledge of the disease.
- Stretching and range of motion exercises
- Exercises to strengthen the abdominal and back muscles
- Correct positions for sleeping and walking
References

Spondylitis Association of America
- Proft F, Poddubnyy D. Ankylosing spondylitis and axial spondyloarthritis: recent insights and impact of new classification criteria. Ther Adv Musculoskelet Dis. 2018 Jun;10(5-6):129-139. [ PMC free article ] [ PubMed ]
- Bridgewood C, Watad A, Cuthbert RJ, McGonagle D. Spondyloarthritis: new insights into clinical aspects, translational immunology and therapeutics. Curr Opin Rheumatol. 2018 Sep;30(5):526-532. [ PubMed ]
- Watad A, Cuthbert RJ, Amital H, McGonagle D. Enthesitis: Much More Than Focal Insertion Point Inflammation. Curr Rheumatol Rep. 2018 May 30;20(7):41. [ PMC free article ] [ PubMed ]
- Mahmoudi M, Garshasbi M, Ashraf-Ganjouei A, Javinani A, Vojdanian M, Saafi M, Ahmadzadeh N, Jamshidi A. Association between rs6759298 and AnkylosingSpondylitis in Iranian Population. Avicenna J Med Biotechnol. 2018 Jul-Sep;10(3):178-182. [ PMC free article ] [ PubMed ]
- van den Berg R, Jongbloed EM, de Schepper EIT, Bierma-Zeinstra SMA, Koes BW, Luijsterburg PAJ. The association between pro-inflammatory biomarkers and nonspecific low back pain: a systematic review. Spine J. 2018 Nov;18(11):2140-2151. [ PubMed ]
- Wang R, Ward MM. Epidemiology of axial spondyloarthritis: an update. Curr Opin Rheumatol. 2018 Mar;30(2):137-143. [ PMC free article ] [ PubMed ]
- Aloush V, Dotan I, Ablin JN, Elkayam O. Evaluating IBD-specific antiglycan antibodies in serum of patients with spondyloarthritis and rheumatoid arthritis: are they really specific? Clin Exp Rheumatol. 2019 Jan-Feb;37(1):32-36. [ PubMed ]
- Rabelo CF, Baptista TSA, Petersen LE, Bauer ME, Keiserman MW, Staub HL. Serum IL-6 correlates with axial mobility index (Bath Ankylosing Spondylitis Metrology Index) in Brazilian patients with ankylosing spondylitis . Open Access Rheumatol. 2018;10:21-25. [ PMC free article ] [ PubMed ]
- Dagfinnrud H, Tidskr nor legefor, 2010
- NICE Guidelines No65
- Rule A, 2017 . Treatment other than biological medicines (EULAR/ASAS recommendations)
- Sepriano A, 2017 . Treatment with biological medicines (EULAR/ASAS recommendations)
- Grans Compendium in Rheumatology





















