Introduction
Psoas syndrome, although often used to describe a series of symptoms related to the muscle of the same name, is not in itself a specific medical diagnosis. Rather, it serves to encompass various potential problems associated with the psoas muscle, located in the abdomen and hip region, playing a crucial role in the movements of the spine and hip.
One of the most common manifestations of psoas syndrome is muscle contracture or tension. Prolonged contraction or excessive tension of the psoas muscle can lead to pain in the lumbar and pelvic region. This pain, often felt as a constant discomfort, can interfere with the quality of daily life of the individual concerned.
Another aspect of psoas syndrome is iliac psoas syndrome. This condition occurs when the psoas muscle irritates the iliac nerve, causing localized pain and discomfort in the hip and lower back region. Symptoms can vary in intensity, from mild pain to more acute and persistent sensations.
Irritation or inflammation of the psoas muscle also represents a facet of the syndrome. This situation can arise from various causes such as injuries, repetitive movements or other triggering factors. When the muscle is irritated or inflamed, it can generate symptoms such as sharp pain, reduced mobility and increased sensitivity in the affected area.
Painful psoas syndrome is a separate condition within this category. Characterized by specific pain associated with the psoas muscle, this syndrome is often triggered by particular movements. Sufferers may experience localized pain during certain physical activities, which may impact their ability to perform normal movements and lead to a reduced quality of life.
Anatomy of the Psoas Muscle
The psoas muscle is one of the most important and complex muscles in the human body. It plays a key role in stabilizing the trunk and enabling lower limb mobility while maintaining intricate functional and anatomical relationships with surrounding structures. A detailed exploration of its origins, insertions, and connections provides a deeper understanding of its fundamental role in human movement and posture.
Origins and Divisions of the Psoas Muscle
The psoas muscle comprises two distinct parts often studied together: the psoas major and the psoas minor (present in approximately 40% of individuals). When paired with the iliacus muscle, they form the iliopsoas group.
- Psoas Major:
- Origin: The psoas major originates on the lateral surfaces of the vertebral bodies, intervertebral discs, and transverse processes of vertebrae T12 to L5. Its fibers converge into a single tendon.
- It extends deeply within the abdominal cavity, descending obliquely towards the pelvic region, where it joins the iliacus muscle.
- Psoas Minor:
- Origin: The psoas minor, when present, arises from the vertebral bodies of T12 and L1 and their intervertebral discs. Unlike the psoas major, it does not cross the hip joint and terminates in a flat tendon.
Insertions of the Psoas Muscle
- The psoas major inserts onto the lesser trochanter of the femur, forming a conjoint structure with the iliacus tendon. This insertion allows the muscle to function as a powerful hip flexor.
- The psoas minor, if present, inserts onto the arcuate line and superior pubic ramus, contributing more to stabilization than mobility.
Anatomical Relationships with Surrounding Structures
The psoas muscle is deeply integrated into the anatomy of the trunk, abdomen, and pelvis, maintaining close relationships with key structures:
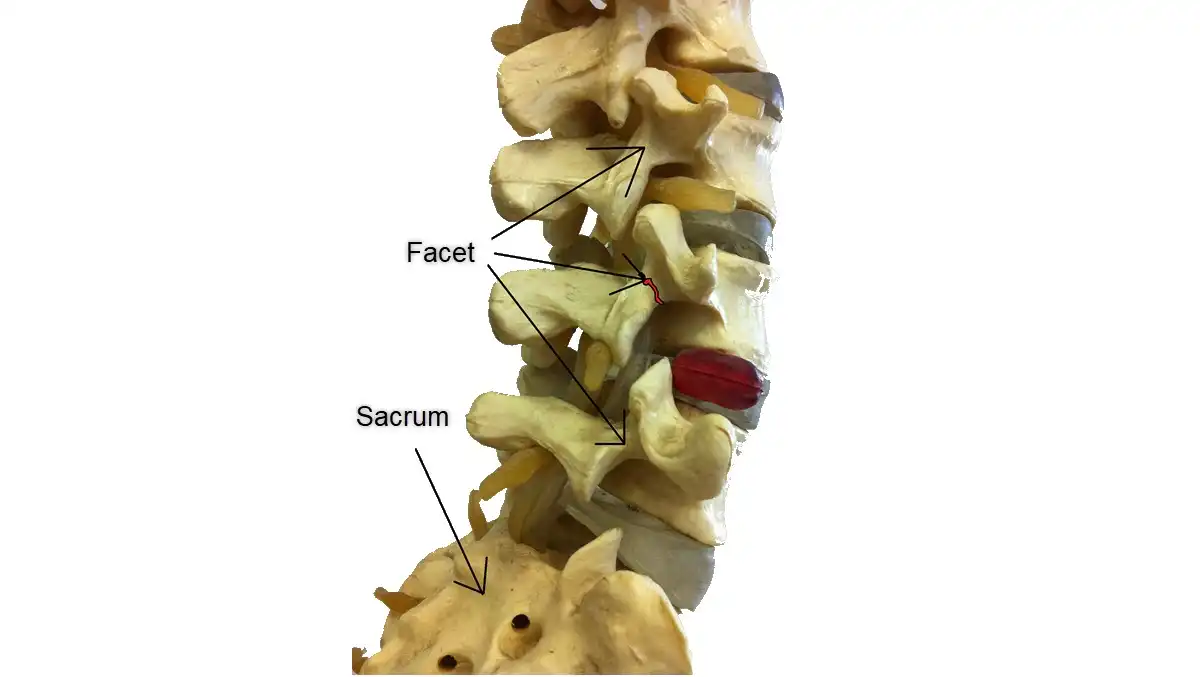
- Spine and Intervertebral Discs:
- Positioned in direct contact with the lumbar vertebral bodies, the psoas is a critical stabilizer of the lumbar spine, aiding in posture and segmental control.
- Nerves and the Lumbar Plexus:
- The lumbar plexus runs through the thickness of the psoas major. Key nerves, such as the femoral, obturator, and ilioinguinal nerves, emerge from the plexus and pass through or around the psoas muscle. Dysfunction in the psoas can lead to nerve compression, causing pain or weakness.
- Diaphragm and Abdominal Structures:
- The upper part of the psoas lies adjacent to the diaphragm, sharing fascial connections. This anatomical relationship influences breathing mechanics and core stability.
- Nearby abdominal organs, including the kidneys, ureters, and intestines, are in close proximity, and the psoas forms part of the retroperitoneal space.
- Pelvic and Hip Structures:
- The psoas passes through the pelvis, forming a critical link between the trunk and lower limbs. Its insertion at the lesser trochanter makes it a pivotal muscle for hip flexion and external rotation.
Functional Role of the Psoas Muscle
- Mobility:
- The psoas major is a primary hip flexor, essential for movements such as walking, running, and climbing stairs.
- It also assists in external rotation and lateral flexion of the trunk.
- Stability:
- The psoas stabilizes the lumbar spine and pelvis during both static postures and dynamic activities.
- It plays a key role in maintaining balance and transferring forces between the upper and lower body.
- Psychosomatic Connections:
- Often referred to as the “muscle of the soul,” the psoas has a unique role in responding to stress and emotional tension, as its deep connections with the diaphragm and spine can influence posture and breathing patterns.
Clinical Relevance
Dysfunction of the psoas muscle can result in a range of issues, including:
Referred pain: In the groin, hip, or even down the leg due to nerve involvement.
Lower back pain: Often linked to tightness or hyperactivity in the psoas, causing compressive forces on the lumbar spine.
Pelvic imbalances: Contributing to asymmetries in gait and posture.
The psoas is actually the union of the psoas major and iliac muscles or iliacus muscle, it is also called iliopsoas muscle or shorter psoas in the jargon of the therapy field.
Iliac muscle : The iliacus arises from the inner part of the pelvic bowl on the upper two-thirds of the iliac fossa and the upper lip of the iliac crest. The iliac muscle then descends into the pelvis and attaches to the lesser trochanter of the femur.
Psoas major muscle : This muscle arises on the front surfaces of the vertebral bodies, intervertebral discs, and transverse processes of the spine, from thoracic level 12 to lumbar level five. It then descends through the pelvis and joins the psoas minor and iliac to insert on the lesser trochanter of your femur.
Psoas minor muscle : The psoas minor arises from the vertebral bodies and discs of the dorsal D12 and lumbar level. It then inserts along the psoas major in an area called the pectineus line and iliac fascia.
Actions of the psoas
- Flex the hip (psoas major and iliacus)
- External rotation of the hip (major and iliac psoas)
- Trunk flexion (psoas major and iliac)
- Tilt the pelvis forward (psoas major and iliacus)
- Helps to laterally flex the lumbar spine (psoas major only)


Causes and Risk Factors of Psoas Syndrome
The psoas muscle plays a vital role in human movement, connecting the lumbar spine to the femur and acting as a key hip flexor and stabilizer. Dysfunction of the psoas muscle, often termed “psoas syndrome,” can result from various causes and is influenced by multiple risk factors. Understanding these underlying issues is critical for effective diagnosis, treatment, and prevention. Below is a detailed discussion of the most common causes and contributing risk factors.
1. Muscle Imbalances
Muscle imbalances are among the leading causes of psoas dysfunction. These occur when the psoas muscle becomes either overactive or underactive in comparison to other muscles involved in hip and core stability.
- Overuse of the Psoas: Activities requiring repeated hip flexion, such as cycling or running, can lead to overuse of the psoas. When the psoas becomes dominant, it compensates for weaker muscles, such as the gluteus maximus or the deep abdominal muscles, leading to tightness and eventual dysfunction.
- Underuse of Supporting Muscles: Prolonged periods of sitting or sedentary behavior can weaken supporting muscles like the hip extensors and core stabilizers. This forces the psoas to take on a disproportionate load, increasing the likelihood of strain.
- Asymmetrical Muscle Development: Uneven muscle strength or flexibility between the left and right sides of the body can place extra stress on the psoas, particularly during activities like running, where one leg may consistently bear more force.
2. Postural Dysfunction
Postural dysfunction is another major contributor to psoas problems. The psoas muscle plays a critical role in maintaining an upright posture and balancing the spine. Poor posture, whether habitual or due to structural issues, can disrupt this function.
- Anterior Pelvic Tilt: A common postural issue where the pelvis tilts forward excessively. This position shortens the psoas, causing chronic tightness and pulling on the lumbar spine.
- Kyphosis or Hyperlordosis: Abnormal curvatures of the spine, such as excessive rounding (kyphosis) or inward arching (hyperlordosis), can alter the alignment of the psoas. This creates uneven tension, leading to discomfort and reduced mobility.
- Prolonged Sitting: Sitting for long periods keeps the psoas in a shortened position, gradually reducing its flexibility. Over time, this adaptation can cause pain and restrict range of motion when standing or walking.
3. Repetitive Strain or Trauma
Repetitive strain and trauma are common triggers of psoas dysfunction, especially in physically active individuals or those with certain occupational demands.
- Overuse Injuries: Repeated movements that engage the psoas, such as high-intensity sports, can cause microtrauma to the muscle fibers. Sports like hurdling, soccer, and martial arts often place excessive strain on the psoas due to rapid hip flexion and rotation.
- Direct Trauma: A fall, car accident, or direct blow to the hip or lower back can damage the psoas muscle or its associated structures, resulting in inflammation, stiffness, and pain.
- Chronic Strain: Activities involving repetitive bending, twisting, or lifting can cause chronic strain, particularly when performed with poor biomechanics or inadequate core support.
4. Risk Factors
Several risk factors increase the likelihood of developing psoas dysfunction. These factors often amplify the effects of the aforementioned causes, making some individuals more susceptible to psoas syndrome.
- Sedentary Lifestyle: Lack of physical activity weakens the core and lower limb muscles, forcing the psoas to compensate. Additionally, prolonged sitting shortens the psoas, predisposing it to tightness and dysfunction.
- Specific Sports or Activities:
- Sports that require repetitive hip flexion, such as cycling, running, and gymnastics, place significant stress on the psoas.
- Activities involving sudden directional changes or kicks, like soccer or martial arts, are also high-risk.
- Poor Ergonomics: Improper workstation setup, such as a poorly positioned desk or chair, encourages slouching and excessive hip flexion. Over time, this contributes to postural dysfunction and muscle imbalances.
- Structural Abnormalities: Leg length discrepancies, scoliosis, or pelvic asymmetry can alter the mechanics of the psoas, leading to overuse or underuse.
- Inadequate Warm-Up or Flexibility: Engaging in physical activity without proper warm-up or stretching can increase tension in the psoas. Limited flexibility reduces the muscle’s ability to perform optimally, heightening the risk of injury.
The Vicious Cycle of Dysfunction
Once the psoas becomes tight or strained, a cycle of dysfunction often ensues. Tightness in the psoas pulls on the lumbar spine, increasing compression and reducing spinal mobility. This leads to compensatory patterns in other muscles and joints, exacerbating imbalances and perpetuating the problem. For instance:
Overcompensation by other muscles, such as the hamstrings or quadratus lumborum, can result in secondary pain or injury.
Tight psoas muscles can inhibit the glutes, leading to further instability in the pelvis and hips.
List of causes
- Muscle tension or contracture: Excessive tension or contracture of the psoas muscle can cause pain and discomfort.
- Iliac nerve irritation: The psoas muscle can put pressure on the iliac nerve, leading to pain in the hip and lower back area.
- Inflammation of the psoas muscle: Injuries, muscle overuse, or repetitive movements can lead to inflammation of the psoas muscle.
- Postural issues: Muscle imbalance or posture issues can affect the psoas muscle and cause symptoms.
- Muscle Injuries: Direct injuries to the psoas muscle, such as strains or tears, can lead to painful symptoms.
- Inflammatory Diseases: Certain inflammatory conditions, such as arthritis, can contribute to problems associated with the psoas.
- Overuse or poor movement habits: Repetitive activities or incorrect movements can contribute to muscle strain.
Symptoms of Psoas Syndrome
Psoas syndrome, characterized by tension or irritation of the psoas muscle, presents with a diverse range of symptoms that can have significant implications on the quality of life of affected individuals. One of the most common signs of this syndrome is lower back pain, localized in the lower back region. This pain may be felt constantly or intermittently and may radiate to the groin or upper thigh. The feeling of stiffness in the lumbar region is also common, limiting mobility and contributing to difficulty in daily activities.
Another symptom associated with psoas syndrome is posture disturbance. Due to the deep location of the psoas muscle and its essential role in stabilizing the spine, its involvement can lead to postural changes. Sufferers may unconsciously adopt compensatory postures to relieve pain, which can lead to muscle imbalances and worsen symptoms of the syndrome.
Psoas syndrome can also manifest as digestive problems. Given the proximity of the psoas muscle to internal organs, its irritation can influence the functioning of the digestive system. Some individuals may experience complaints such as bloating, abdominal heaviness or intestinal problems, highlighting the complexity of the symptoms associated with this syndrome.
Impaired mobility is another significant symptomatic aspect of psoas syndrome. Affected individuals may experience decreased flexibility in the hip, which may result in difficulty performing movements such as bending or extending the leg. These limitations can impact daily activities, whether it’s climbing stairs, bending, or even walking comfortably.
Additionally, psoas syndrome can influence the emotional well-being of affected individuals. Persistent pain and disruption to daily activities can lead to stress and anxiety. Likewise, the physical restrictions caused by the syndrome can impact sleep quality, exacerbating emotional problems and creating a vicious cycle of pain and distress.
It is essential to note that the symptoms of psoas syndrome can vary from person to person in intensity and combination. Some individuals may experience primarily lower back pain, while others may experience a broader range of symptoms. Accurately diagnosing psoas syndrome requires a thorough evaluation by a healthcare professional, often an osteopath or physiotherapist, to design a personalized treatment plan.
List of symptoms
- Lower back pain: Pain in the lumbar region (lower back) is commonly associated with psoas syndrome.
- Hip pain: Symptoms may include pain or discomfort in the hip area, especially during specific movements.
- Pain or tightness in the groin: Some people may feel pain or discomfort in the groin area, which may be related to irritation or tightness of the psoas muscle.
- Feeling of stiffness or tension in the lower back: In addition to lower back pain, some people may feel stiffness or tension in the lower back region, often associated with limitation of movement.
- Feeling of pelvic imbalance or instability: Psoas syndrome can disrupt pelvic balance and cause a feeling of imbalance or instability when walking or rotating the trunk.
- Radiating Thigh Pain: In some cases, pain associated with psoas syndrome may radiate down the thigh, causing additional discomfort when walking or other activities.
- Feeling of muscle weakness: Tension or irritation of the psoas muscle can sometimes lead to a feeling of weakness in the lumbar region or hip, affecting the ability to perform normal movements.
- Pain in the lower abdomen: Some people experience pain or tightness in the lower abdomen.
- Difficulty walking: Symptoms such as difficulty walking or making hip movements may be present.
- Pain with prolonged sitting: Pain may worsen with prolonged periods of sitting.
- Limited hip movements: A feeling of stiffness or limitations in hip movements may be observed.
- Pain during certain activities: Symptoms may be triggered or worsened by specific activities, such as walking, running, or climbing stairs.
- Pain during trunk rotation activities: Trunk rotation movements may worsen pain or discomfort in the lower back or hip area in some people with psoas syndrome.
- Pain during forward bending: Forward bending, such as bending over to pick something up, can trigger or worsen pain in people affected by this syndrome.
- Sensation of abdominal compression: Some individuals may feel a sensation of compression or pressure in the abdominal area, often associated with tightness of the psoas muscle.
- Pain while lying on your back: In some people, pain may be worse when lying on their back, due to the increased strain on the psoas muscle in this position.
- Pain while sitting with legs extended: Pain can also be exacerbated when the legs are extended while sitting, due to increased tension on the psoas muscle.
Impact of Increased Psoas Tension on Lumbar Curvature
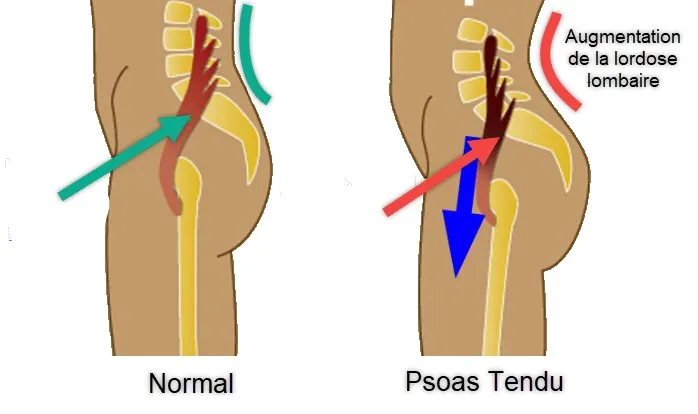
Increased psoas muscle tension can exert a significant influence on lumbar curvature, thus playing a crucial role in the development of various postural and lumbar problems. The psoas, a deep muscle located in the lumbar region, is essential for maintaining spinal stability and is directly related to the natural lumbar curvature. When this muscle becomes tight or contracted, it can cause an imbalance in the lumbar region, influencing the natural curvature of the spine.
Increased tension in the psoas muscle can lead to an anterior tilt of the pelvis, a phenomenon known as anterior pelvic tilt. This occurs when the psoas muscle pulls excessively on the pelvis, causing it to tilt forward. As a result, this anterior tilt can contribute to increased lumbar curvature, creating excessive lordosis.
Excessive lordosis, characterized by an accentuated curvature in the lumbar region, can lead to significant postural and lumbar problems. In addition to lower back pain, this increased curvature can affect load distribution across the spine, increasing stress on the spinal discs and lumbar joints. This can contribute to the development of conditions such as herniated discs and spinal stenosis.
The impact on lumbar curvature can also influence overall posture. Excessive lordosis can result in forward projection of the shoulders, increased thoracic curvature, and a forward positioned head. These compensatory adjustments can lead to a range of postural problems, affecting not only the spine but also the joints of the upper limbs.
Increased psoas tension can also affect opposing muscles, such as the abdominal muscles. Due to the antagonistic muscular relationship between the psoas and the abdominals, a tight psoas can weaken the abdominal muscles, further worsening the muscle imbalance. Decreased abdominal strength can compromise core stability, contributing to excessive lumbar lordosis.
The consequences of increased psoas tension go beyond the physical aspects. Psychosocial implications may also arise, as chronic low back pain and postural alterations can affect quality of life and emotional well-being. Individuals may experience stress, anxiety, and limitations in daily activities due to pain and movement restrictions.
To counter the negative influence of psoas tension on lumbar curvature, targeted treatment approaches are necessary. Psoas stretching and release techniques can be used to relieve muscle tension. Strengthening the abdominal muscles and core stabilizing muscles can help restore muscular balance, promoting healthy posture.
- Anterior Pelvic Tilt: When the psoas is tight, it can pull on the spine, causing an anterior pelvic tilt. This can accentuate the natural curve of the lumbar region, leading to excessive lordosis, also called hyperlordosis.
- Postural Compensation: Increased psoas tension can lead to postural compensation. To counter psoas pull, the body may respond by increasing lumbar curvature, creating an unbalanced posture.
- Stress on Intervertebral Discs: Increased lumbar curvature due to increased psoas tension can place additional pressure on the intervertebral discs in the lumbar region. This can potentially contribute to problems such as lower back pain, degenerative discs, or other spinal-related disorders.
- Altered Pelvic Alignment: The psoas is attached to the pelvic region, and excessive tension can influence pelvic alignment. This can disrupt the muscular balance around the lumbar spine, contributing to excessive curvature.
Psoas Syndrome vs. Myofascial Psoas Syndrome
“Psoas syndrome” and “Myofascial Psoas Syndrome” are terms that can sometimes be used interchangeably, although their meaning can vary depending on the context and understanding of those using them.
- Psoas Syndrome: This term is often used generally to describe symptoms related to the psoas muscle. Symptoms may include lower back pain, hip pain, difficulty walking, and other discomforts associated with this muscle. However, it may be a generic term used to describe various psoas conditions without specifying a particular cause.
- Myofascial Psoas Syndrome: Myofascial syndrome generally refers to trigger points in the muscle and connective tissue (fascia) that can cause pain and tension. Thus, “psoas myofascial syndrome” could indicate a condition where trigger points in the psoas muscle lead to specific symptoms. Trigger points can be hypersensitive, knotty areas in the muscle that can cause pain locally or refer to other areas of the body.

Exploring Liz Koch’s Insights on the Psoas
Liz Koch, an American movement expert and author, has distinguished herself for her extensive work on the psoas. His fame stems from his exploration of the role of the psoas in physical and emotional well-being. Through her book titled “The Psoas Book,” she generously shares her knowledge about this muscle, highlighting its crucial impact on posture, movement and overall health.
The psoas, often referred to as the ” muscle of the soul ” or the ” muscle of emotions “, depending on certain contexts, is at the heart of Liz Koch’s concerns.
She puts forward the idea that this muscle can play a role in releasing emotional tension stored in the body.
Focusing on the connection between the psoas and the nervous system, she points out that tension in this muscle can be linked to past emotional experiences.
Liz Koch’s suggestions include techniques and exercises aimed at increasing awareness of the psoas, releasing tension and promoting natural movement of the body. His ideas have had a significant influence on many movement practitioners, particularly in the fields of yoga, dance and kinesiology.
It is essential to note that although Liz Koch’s perspectives on the psoas and its connection to emotions may be considered alternative medicine, they are not necessarily validated by conventional scientific evidence. Despite this, his work has captured attention and helped raise awareness of the importance of the psoas in physical and emotional health. If these concepts intrigue you, exploring the writings and teachings of Liz Koch might offer a deeper understanding.
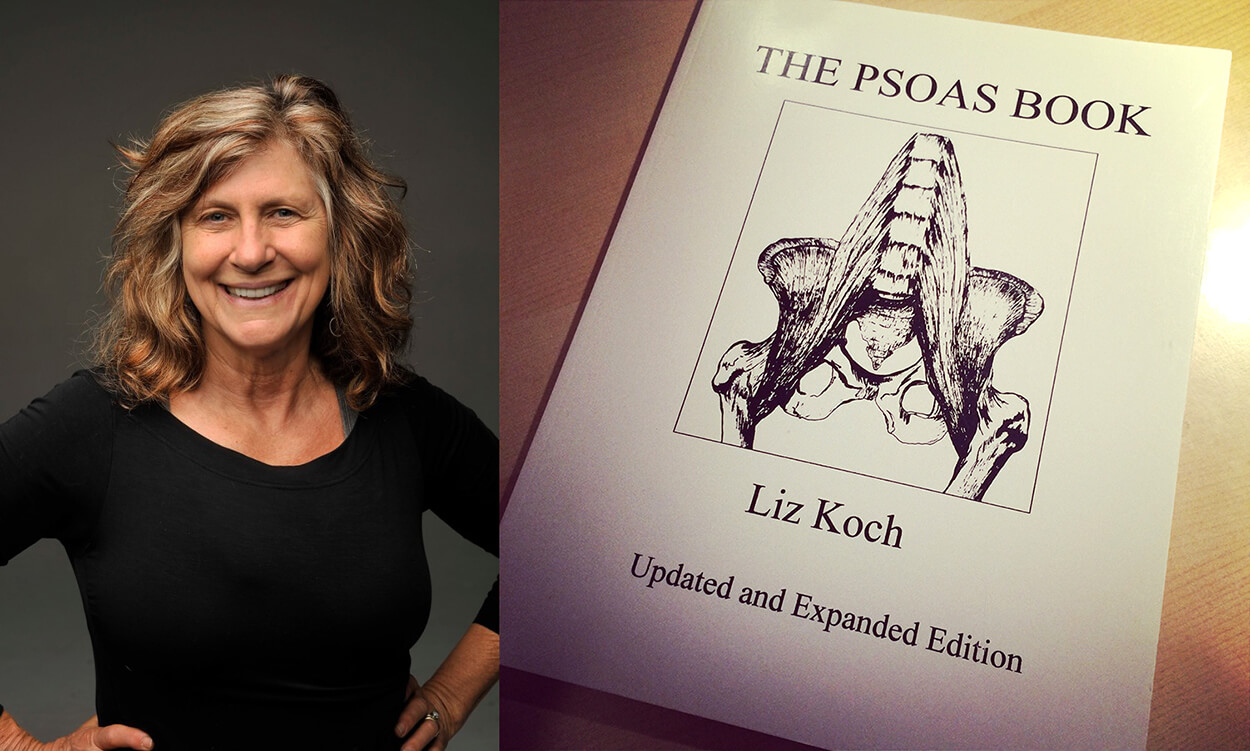
“The only muscle that connects your spine to your leg, the psoas, is much of the source of lower back discomfort and anxiety with orgasmic pleasure. “
Liz Koch,
She adds:
» A tight psoas can disrupt digestion, reproduction and create a host of other discomforts. “
Psoas syndrome is characterized by pain in the lower back, which radiates down one leg, making it difficult to maintain correct posture. Although this syndrome is often found in those suffering from low back pain, it is largely forgotten by therapists.
The Visceral Psoas Connection: Anatomy, Function, and Emerging Perspectives
The psoas muscle, often referred to as the “muscle of the soul” in some alternative health circles, is more than just a key player in hip and spinal mechanics. Emerging theories suggest it has deeper connections to the visceral system and the autonomic nervous system (ANS), potentially linking it to emotional health and overall well-being. While scientific research on this subject is still limited, the anatomical position and function of the psoas make it a compelling topic for exploration.
Anatomy and Function of the Psoas
The psoas muscle is a deep-seated structure that originates from the lumbar vertebrae (T12-L5) and inserts into the lesser trochanter of the femur. It crosses the pelvis and serves as a major hip flexor, playing a critical role in activities like walking, running, and stabilizing the spine. The psoas is part of the iliopsoas group, which includes the iliacus muscle.
Anatomically, the psoas is uniquely positioned in the body:
- Close Proximity to Organs: The psoas lies adjacent to the abdominal cavity and is in contact with several internal organs, including:
- The kidneys.
- The intestines (small and large bowel).
- The adrenal glands.
- Major blood vessels, such as the abdominal aorta and inferior vena cava.
- Neural Connections: The psoas has rich innervation from the lumbar plexus, a network of nerves that also supply sensory and motor input to the abdominal and pelvic regions.
These features make the psoas a potential mediator between musculoskeletal, visceral, and autonomic systems.
The Visceral Connection
The “visceral psoas connection” refers to the idea that the psoas interacts with the internal organs and the autonomic nervous system due to its anatomical proximity and shared neural pathways. Some practitioners argue that tension in the psoas could influence or be influenced by visceral health. Key aspects of this theory include:
- Fascial Continuity: The psoas is enveloped by the deep fascia, which is continuous with the fascia surrounding internal organs. This continuity might allow mechanical tension in the psoas to affect organ mobility or function and vice versa.
- Sympathetic and Parasympathetic Influence: The psoas is located near the sympathetic ganglia of the lumbar spine. Stress or tension in this region could theoretically influence autonomic regulation, potentially impacting digestion, circulation, and other visceral functions.
- Emotional Storage Hypothesis: Pioneered by movement educator Liz Koch, the idea that the psoas stores emotional stress has gained popularity in holistic and alternative health communities. According to this perspective, chronic tension in the psoas may result from unresolved trauma or stress, which can manifest in physical symptoms such as digestive issues or pelvic discomfort.
Emotional and Stress-Related Connections
The idea that the psoas is influenced by emotions stems from its relationship with the autonomic nervous system. Chronic stress can activate the sympathetic nervous system (fight-or-flight response), leading to tension in muscles, including the psoas. Over time, this tension may become ingrained, contributing to discomfort and dysfunction.
Proponents of this theory suggest that:
- Emotional Triggers: Past emotional experiences, particularly traumatic ones, may leave an imprint on the psoas through nervous system pathways.
- Mind-Body Practices: Techniques such as yoga, somatic therapy, and myofascial release often target the psoas to address both physical and emotional tension.
While these claims are primarily anecdotal, they highlight the potential for a holistic approach to psoas-related issues.
Challenges in Scientific Validation
Although the visceral and emotional connection of the psoas is a fascinating concept, it remains largely within the realm of alternative medicine. Scientific research on the topic is limited for several reasons:
- Complexity of the Psoas: Its deep location and multifaceted role in the body make it challenging to study in isolation.
- Subjectivity of Emotional Experiences: Emotional connections to physical structures are difficult to measure objectively, relying heavily on patient-reported outcomes.
- Skepticism in Medicine: Mainstream medicine often prioritizes structural and biomechanical explanations over more integrative or holistic models.
Clinical Implications and Therapeutic Approaches
Whether or not the visceral psoas connection is scientifically validated, it offers valuable insights for practitioners working with patients experiencing chronic pain or stress-related conditions. Approaches that consider both the physical and emotional aspects of the psoas include:
Holistic Assessments: Considering the role of visceral health and posture can provide a more comprehensive understanding of psoas-related issues.
Manual Therapy: Techniques such as osteopathic manipulation, trigger point therapy, and myofascial release can address physical restrictions in the psoas.
Movement Practices: Yoga, pilates, and somatic exercises help lengthen and release tension in the psoas while promoting relaxation and body awareness.
Stress Management: Mindfulness, breathing exercises, and psychotherapy can complement physical interventions by addressing underlying emotional factors.
Exploring the Emotional Aspect of the Psoas
The psoas muscle, often described as the “emotion muscle” in alternative wellness circles, is more than just a key player in physical movement. Positioned deep within the body, the psoas spans from the lumbar spine to the femur and is fundamental to activities such as walking, running, and maintaining posture. However, beyond its biomechanical role, some practitioners and movement experts, such as Liz Koch, suggest that the psoas holds an emotional dimension, acting as a physical repository for stress and unresolved trauma.
While these ideas are not yet widely validated within conventional scientific frameworks, they are embraced in holistic and alternative medicine, forming the basis for a deeper exploration of the connection between the mind and body.
The Emotional Role of the Psoas
The emotional aspect of the psoas centers on its purported connection to the autonomic nervous system (ANS), which governs the body’s stress response. This theory posits that the psoas muscle, given its location and neural connections, plays a dual role: physical stabilization and emotional regulation.
- Autonomic Nervous System Connection:
- The psoas lies near the sympathetic trunk, a network of nerves associated with the fight-or-flight response. Chronic stress or trauma may trigger hyperactivity in the sympathetic nervous system, potentially leading to persistent tension in the psoas.
- Conversely, relaxation of the psoas is theorized to engage the parasympathetic nervous system, fostering a sense of calm and safety.
- Storage of Emotional Memory:
- Advocates of this perspective argue that emotional experiences, particularly traumatic events, can leave an imprint on the body through muscle tension. The psoas, as a core muscle linked to survival mechanisms, may contract during stress and fail to fully relax once the immediate threat has passed.
- Over time, this unresolved tension is thought to manifest as physical discomfort, restricted movement, or even anxiety and emotional distress.
- Somatic Experiences:
- The psoas is considered a bridge between the upper and lower body, making it central to physical alignment and grounding. Holistic practitioners often associate this muscle with the concept of “core emotional stability,” suggesting that tension in the psoas reflects feelings of vulnerability, fear, or insecurity.
Manifestations of Emotional Tension in the Psoas
Emotional tension in the psoas may manifest as a combination of physical and psychological symptoms:
- Physical Symptoms:
- Chronic low back pain.
- Tightness or discomfort in the hips or pelvis.
- Poor posture or difficulty maintaining an upright stance.
- Limited range of motion, particularly in the hips.
- Emotional Symptoms:
- Feelings of unease, anxiety, or restlessness.
- Emotional reactivity or heightened sensitivity.
- Difficulty “letting go” of past experiences or feelings of being “stuck.”
These manifestations highlight the potential interplay between physical tension in the psoas and emotional well-being, suggesting that addressing one aspect could positively influence the other.
Approaches to Releasing Emotional Tension in the Psoas
A variety of holistic and somatic practices aim to release tension in the psoas, with the broader goal of improving both physical and emotional health. While these methods often lack rigorous scientific backing, they have been widely reported to promote relaxation and stress relief.
- Myofascial Release:
- Myofascial release targets the fascia surrounding the psoas and other muscles. Through gentle, sustained pressure, this technique aims to alleviate physical restrictions and promote relaxation.
- Somatic Movement Practices:
- Practices like yoga, pilates, and somatic therapy often include poses and movements designed to lengthen and release the psoas.
- Poses such as the reclining bound angle pose or lunge stretches are frequently used to target the psoas while encouraging mindfulness and relaxation.
- Breathwork:
- Deep, diaphragmatic breathing is thought to influence the psoas by engaging the diaphragm, a muscle closely connected to the psoas through fascial structures.
- Breathwork practices aim to calm the nervous system, facilitating relaxation in both the psoas and the body as a whole.
- Trauma-Informed Bodywork:
- Therapies like TRE (Tension and Trauma Releasing Exercises) focus on gentle shaking or tremoring movements that may help release deep-seated tension in the psoas and other muscles.
- Mindful Awareness:
- Mind-body practices emphasize cultivating awareness of the psoas and its tension patterns. By developing a greater sense of connection to this area, individuals may begin to release emotional and physical stress.
The Debate: Science vs. Holistic Perspectives
It is important to note that the emotional dimension of the psoas is largely anecdotal and resides within the realm of alternative and holistic medicine. While proponents like Liz Koch highlight its role in emotional well-being, mainstream scientific research has yet to fully explore or validate these claims.
Skeptics argue that without empirical evidence, the emotional aspect of the psoas remains speculative. However, holistic practitioners counter that anecdotal evidence and the lived experiences of individuals provide meaningful insights that warrant further investigation
Integrating the Emotional and Physical Aspects
Whether viewed through a scientific lens or a holistic framework, addressing the psoas as both a physical and emotional structure can offer a well-rounded approach to health. For individuals experiencing chronic tension or stress, combining traditional therapies with mindfulness-based practices can provide a comprehensive path to healing.
For example, an osteopath or physiotherapist might focus on structural imbalances in the psoas, while a yoga instructor might guide practices to release emotional tension. Together, these approaches could complement one another, offering relief on multiple levels.
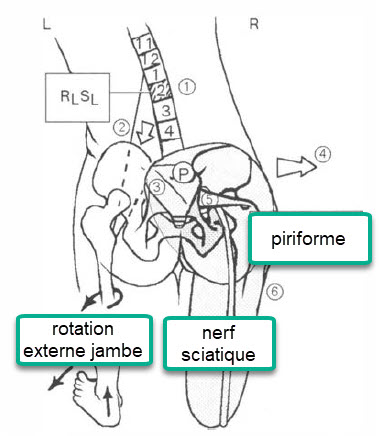
Clinical Presentation of Psoas Syndrome
Patients often complain of back pain in the lumbosacral region. Radiation downward into the sacrum or upward into the lumbar vertebra may occur – the location of the pain is described as buttock pain, pelvic pain or groin pain. The patient may report a catching or sliding sensation in the groin when their knee is flexed 90 degrees. Pain and a “blocking” sensation in the groin when the knee is flexed to 90 degrees suggests a labral tear but may also be seen in iliopsoas tendinopathy.
The patient is bent forward, leaning to the left side and the left foot is turned out.
include:
- Non-neutral key somatic dysfunction in L 1 or L2 which is curved laterally to the left,
- Marked spasm of the left psoas muscle.
- Rotation of the sacrum on a left oblique axis (often of the non-neutral type).
- Right pelvic lateral shift.
- Right piriformis spasm
- Pain in right hip, back of right leg, but not usually past knee.
Differential diagnoses of Psoas syndrome
- Tendonitis or Muscle Injury: Damage or inflammation to other muscles in the abdominal area or hip can lead to symptoms similar to psoas syndrome.
- Appendicitis: Inflammation of the appendix can cause pain in the right abdominal area, sometimes confused with symptoms of psoas syndrome.
- Renal Colic: Kidney stones can cause sharp pain in the lower back and abdominal area, resembling that of psoas syndrome.
- Inguinal Hernia: An inguinal hernia can cause pain in the groin and lower abdomen area, sometimes overlapping with the symptoms of psoas syndrome.
- Endometriosis: In women, endometriosis can cause pelvic pain that can be confused with symptoms of psoas syndrome.
- Colitis: Inflammatory bowel diseases, such as colitis, can cause lower abdominal pain similar to psoas syndrome.
- Spinal Problems: Spinal disorders, such as herniated discs or joint problems, can also cause pain in the lumbar region.
- Irritable Bowel Syndrome (IBS): IBS can cause abdominal pain, bloating, and changes in bowel habits, which can be confused with symptoms of psoas syndrome.
Assessment Tests for Screening Psoas Syndrome
Thomas’ test
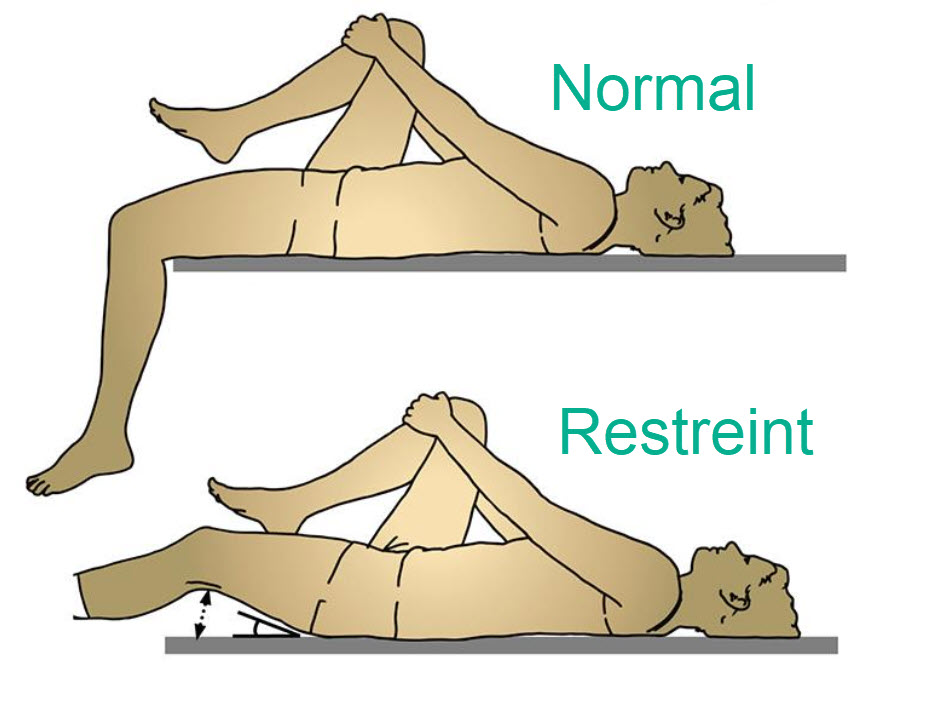
The Thomas test, also known as the psoas test, is an orthopedic examination that aims to assess the length and flexibility of the iliopsoas muscle. This test is often used in the medical and physical therapy fields to evaluate potential dysfunctions of the psoas muscle.
Here is how the Thomas test is typically performed:
- The patient lies on an examination table with his back against the table.
- Both of the patient’s knees are pulled toward the chest, allowing the back to make full contact with the table.
- One knee is then released to hang along the side of the table, while the other knee remains pulled toward the chest.
- The practitioner observes the position of the hanging thigh to assess for the presence of deviations or elevations, which may indicate tension or contraction of the iliopsoas muscle.
If the hanging thigh shows significant elevation relative to the table, this may suggest contraction of the psoas muscle. Abnormal results may indicate restricted mobility or imbalances in the psoas muscle.
Check the strength of your psoas
If you are able to raise your knee 90 degrees, your psoas is working well
Therapeutic Approaches
1. Counterstrain psoas major

To treat the psoas major muscle with the Counterstrain technique, the practitioner will often follow these steps:
- Patient Positioning: The patient is placed in a specific position that allows the psoas muscle to relax. Often this involves placing the patient on their side with their knees bent, so as to minimize strain on the psoas.
- Trigger point identification: The practitioner uses a palpatory technique to identify sensitive trigger points in the psoas major muscle.
- Muscle positioning: The practitioner positions the muscle in a position where it is shortened and relaxed, which can help reduce tension.
- Maintaining the position: The practitioner holds the position for a short period of time, usually 90 seconds to a few minutes. This allows the muscle to relax and reduce tension.
- Gradual return to neutral position: The practitioner then guides the patient gradually to return to a neutral position.
2. Counterstrain psoas minor

Ipsilateral hip flexion
3. Iliac


Place the unaffected leg on top of the affected leg, flex both legs at the hip, externally rotate both legs, lower the knees (frog legs).
Muscle stretching
Start with a kneeling psoas stretch.
- Drop your left knee underneath you, with your left leg extending away from your body and your toes touching the floor.
- Place your right leg in front of you (your foot flat on the floor), so that your right leg forms at a 90-degree angle.
- Using the strength of your buttock, gently bring your left knee back. As you do so, maintain good posture with your shoulders high and your head straight. Hold this position for 30 seconds, then repeat on the opposite leg.

Bridge Pose
Bridge pose, also known as Setu Bandhasana in yoga, can be beneficial for stretching and strengthening the psoas muscle. Here’s how to perform bridge pose to target psoas stretching:
- Starting position: Lie on your back with your knees bent and your feet hip-width apart. The arms should be alongside the body, palms down.
- Foot placement: Position your feet so that they are in line with your knees, with your toes pointing forward.
- Abdominal Engagement: Activate your abdominal muscles by pressing your lower back into the floor. This will help stabilize the spine.
- Hip Raise: As you inhale, begin to slowly raise your hips toward the ceiling, pushing through both your feet and arms. Continue to press your lower back into the floor.
- Forming a straight line: Form a straight line from the shoulders to the knees when the hips are up. Avoid arching your back too much.
- Maintain posture: Hold the position for 30 seconds to 1 minute, breathing deeply and continuing to activate the abdominal muscles.
- Lower yourself slowly: Exhale and slowly lower your hips downward, vertebra by vertebra, until your back is completely on the floor.
Additional Tips:
- Avoid overextending your neck by keeping your chin toward your chest.
- For a more pronounced psoas stretch, you can try gently walking your feet forward while maintaining bridge pose.
This pose helps open and stretch the muscles in the front of the thigh, including the psoas. As with any yoga practice, listen to your body, don’t force it, and adapt the pose according to your needs and comfort level. If you have back problems or other medical concerns, consult a healthcare professional before practicing this pose.

Warrior pose
Warrior Pose (Virabhadrasana) is a yoga posture that can help stretch the psoas muscle, in addition to strengthening the legs, arms and core. Here’s how to do Warrior Pose I, which specifically targets the psoas:
- Starting position: Start in a standing position with your feet together.
- Spread your feet: Spread your feet about hip-width apart.
- Feet orientation: Orient the right foot forward and the left foot slightly inward (approximately 45 degrees).
- Hip Alignment: Make sure your hips are facing forward.
- Knee Flexion: Bend the right knee, ensuring that the knee is directly above the ankle.
- Psoas Stretch: As you bend your right knee, you should feel a stretch along the psoas on your left side.
- Arms straight: Extend your arms overhead with your palms facing each other.
- Hold the pose: Hold the pose for 30 seconds to 1 minute, breathing deeply.
- Switch sides: Return to the starting position and repeat on the other side, bending the left knee.

Advice :
- Keep your trunk straight and engage your abdominal muscles to maintain stability in the posture.
- Make sure the flexed knee is aligned with the ankle to avoid unnecessary stress on the knee joint.
- Breathe deeply to help relax and stretch the psoas.
Warrior Pose is a powerful pose that can also strengthen the legs, improve balance and boost energy. However, if you have knee, hip, or back problems, consult a healthcare professional or yoga instructor for modifications tailored to your physical condition.
External rotation of the femur
Simply internally rotating your back leg while doing the half-kneeling psoas stretch works your entire psoas muscle more effectively.
To use this modification, move the foot of your back leg toward the other side of your body. Your back leg should be diagonally behind you rather than straight back. This will rotate your leg inward.
Hold the stretch for 30 seconds, then switch to the other side.
Combine the psoas stretch with the quadriceps stretch
Lift the foot of your back leg toward your butt as you stretch the psoas to half-kneeling.
References
- Sutherland WG. Teachings in the Science of Osteopathy. Portland, OR: Rudra Press; 1990:279-281.Dydyk AM, Sapra A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Nov 2, 2021. Psoas Syndrome. [PubMed]
- Tyler TF, Fukunaga T, Gellert J. Rehabilitation of soft tissue injuries of the hip and pelvis. Int J Sports Phys Ther. 2014 Nov;9(6):785-97. [PMC free article] [PubMed]
- Tsukada S, Niga S, Nihei T, Imamura S, Saito M, Hatanaka J. Iliopsoas Disorder in Athletes with Groin Pain: Prevalence in 638 Consecutive Patients Assessed with MRI and Clinical Results in 134 Patients with Signal Intensity Changes in the Iliopsoas. JB JS Open Access. 2018 Mar 29;3(1):e0049. [PMC free article] [PubMed]
- Anderson CN. Iliopsoas: Pathology, Diagnosis, and Treatment. Clin Sports Med. 2016 Jul;35(3):419-433. [PubMed]
- Thomas E, Cavallaro AR, Mani D, Bianco A, Palma A. The efficacy of muscle energy techniques in symptomatic and asymptomatic subjects: a systematic review. Chiropr Man Therap. 2019;27:35. [PMC free article] [PubMed]
- ollins CK, Masaracchio M, Cleland JA. The effectiveness of strain counterstrain in the treatment of patients with chronic ankle instability: A randomized clinical trial. J Man Manip Ther. 2014 Aug;22(3):119-28. [PMC free article] [PubMed]
- Bordoni B, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 21, 2021. Anatomy, Bony Pelvis and Lower Limb, Iliopsoas Muscle. [PubMed]
- Hu H, Meijer OG, van Dieën JH, Hodges PW, Bruijn SM, Strijers RL, Nanayakkara PW, van Royen BJ, Wu WH, Xia C. Is the psoas a hip flexor in the active straight leg raise? Eur Spine J. 2011 May;20(5):759-65. [PMC free article] [PubMed]