Introduction
Lumbar lordosis is a term used to describe the natural inward curvature of the lumbar spine, which is the lower portion of the vertebral column located in the lower back. This curvature is essential for maintaining balance, absorbing shock, and allowing for flexibility and movement in the lower back region. Lumbar lordosis helps distribute body weight evenly along the spine, reducing the risk of injury and strain.
The lumbar spine normally has a slight lordotic curve, which is more pronounced in some individuals than in others. This curvature is formed by the shape of the vertebrae, the intervertebral discs, and the surrounding ligaments and muscles. In a healthy spine, the lordotic curve is balanced and aligned, providing stability and support for the upper body and pelvis.
However, abnormalities or excessive curvature of the lumbar lordosis can lead to various issues and discomfort. Hyperlordosis, or excessive inward curvature of the lumbar spine, can result in lower back pain, muscle tightness, and postural problems. It may be caused by factors such as poor posture, muscle imbalances, obesity, pregnancy, or certain medical conditions such as spondylolisthesis or osteoporosis.
Conversely, hypolordosis, or a reduction in the normal lumbar curvature, can also cause problems. It may lead to decreased flexibility, limited range of motion, and increased pressure on the spinal discs and joints. Hypolordosis is often associated with conditions such as flatback syndrome, ankylosing spondylitis, or degenerative disc disease.
Treatment for abnormal lumbar lordosis depends on the underlying cause and severity of the condition. For hyperlordosis caused by muscle imbalances or poor posture, physical therapy exercises focusing on strengthening the core muscles and stretching tight muscles can help correct the curvature and alleviate symptoms. Weight management, ergonomic adjustments, and lifestyle modifications may also be recommended to reduce strain on the lower back.
Evolution of Lumbar Lordosis
Role in Human Bipedalism
Lumbar lordosis, this natural curve of the spine, played a fundamental role in the evolution of humans towards bipedalism. Even before hyperlordosis was a concern, lumbar lordosis was crucial to our ability to walk upright.
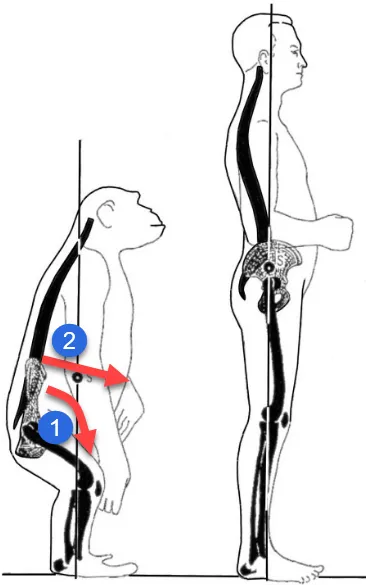
When our ancestors evolved to adopt a bipedal posture, the spine underwent notable adaptations to support this new way of moving. The natural curve in the lumbar region was essential for maintaining balance, distributing body weight efficiently, and enabling stable bipedal locomotion.
This curvature allowed the spine to act as a spring, absorbing shock while walking and contributing to the agility needed for hunting and avoiding predators. Lumbar lordosis has therefore been an evolutionary advantage, favoring the survival and success of our species.
However, in our modern lifestyle this curvature can sometimes become excessive, leading to problems such as hyperlordosis. It is essential to understand the line between healthy and excessive curvature, because too much lumbar lordosis can lead to orthopedic complications.
By exploring the evolution of lumbar lordosis, we can better understand how our anatomy adapted to allow us to become agile bipeds. At the same time, it highlights the importance of maintaining balance in our posture to prevent spine-related health problems in our modern life.
Impact of Modern Sedentary Lifestyle
The appearance of hyperlordosis, excessive curvature of the spine in the lumbar region, could be attributed to significant changes in the lifestyle of modern man. If we go back in time, our ancestors adopted a natural bipedal posture, with a lumbar lordosis adapted to walking and running.
However, with the advent of an increasingly sedentary society, marked by a reduction in physical activities, the impact on human posture has been significant. Less effort when running, excess weight and a less active lifestyle can contribute to an increase in lumbar curvature.
Reducing physical activity weakens the muscles that support the spine, especially those in the lumbar region. At the same time, excess weight placed on the spine can accentuate the natural curvature, possibly leading to hyperlordosis.
This change in muscle dynamics and imbalance caused by a sedentary lifestyle can create excessive strain on the spine. Weakened lower back muscles and excess weight can contribute to increased curvature, creating the conditions for hyperlordosis.
Thus, by examining the implications of sedentary lifestyle on human posture, we can better understand how modern factors may contribute to orthopedic problems such as hyperlordosis.
Causes of lumbar lordosis
Lumbar lordosis, a natural inward curvature of the lower spine, is essential for balance, flexibility, and shock absorption. However, when this curve becomes exaggerated, known as hyperlordosis, or diminished, referred to as hypolordosis, it can lead to discomfort, reduced mobility, and other complications. Understanding the causes of lumbar lordosis is critical for prevention and treatment. Below, we delve into the primary contributing factors.
Poor Posture
One of the most common causes of lumbar lordosis is poor posture. Spending extended periods sitting improperly, slouching, or standing with excessive pelvic tilt can gradually alter the natural curvature of the spine. Modern lifestyles, dominated by desk jobs, prolonged use of electronic devices, and reduced physical activity, exacerbate these postural issues. Over time, muscles in the lower back become tight, and the abdominal muscles weaken, resulting in an imbalance that accentuates the lumbar curve.
Correcting poor posture requires conscious effort and ergonomic adjustments. Using lumbar-supportive chairs, maintaining an upright sitting position, and incorporating posture-correcting exercises can help prevent or mitigate the impact of poor posture on lumbar lordosis.
Obesity and Pregnancy
Excess weight, particularly around the abdominal area, shifts the body’s center of gravity forward, increasing the strain on the lower back. This can lead to an exaggerated lumbar curve as the spine adjusts to support the additional weight. Obesity not only alters posture but also weakens the core muscles, which are essential for spinal stability.
Similarly, pregnancy is a significant contributor to temporary hyperlordosis. As the fetus grows, the additional weight in the abdominal region shifts the pelvis forward, increasing lumbar curvature. Hormonal changes during pregnancy, such as the release of relaxin, can further affect the stability of ligaments and joints, compounding the strain on the lower back.
In both cases, weight management through a balanced diet, regular physical activity, and targeted exercises can alleviate stress on the lumbar spine. For pregnant individuals, prenatal yoga and other low-impact exercises can help maintain spinal health.
Muscle Imbalances
The alignment and curvature of the spine depend heavily on the balance between the muscles in the core, back, and hips. When this balance is disrupted, it can lead to hyperlordosis. Weak abdominal muscles, tight lower back muscles, and shortened hip flexors are common culprits.
Muscle imbalances often arise from repetitive motions, improper exercise techniques, or prolonged periods of inactivity. For instance, athletes who focus solely on strengthening the back without equally working on the core may unintentionally create an imbalance. Similarly, individuals with sedentary lifestyles may develop tight hip flexors and weak glutes, which alter pelvic alignment and increase lumbar curvature.
Addressing muscle imbalances involves targeted exercises that strengthen weak muscles and stretch tight ones. Core stabilization exercises, hip flexor stretches, and lower back flexibility routines are often recommended to restore balance and improve posture.
Neurological and Genetic Factors
Certain neurological conditions and genetic predispositions can also contribute to abnormal lumbar lordosis. Disorders such as muscular dystrophy, cerebral palsy, and polio affect muscle tone and coordination, often resulting in postural changes, including excessive curvature of the lumbar spine. These conditions can weaken the muscles supporting the spine, making it more challenging to maintain proper alignment.
Genetic factors, such as congenital spinal abnormalities or a naturally exaggerated lumbar curve, may also predispose individuals to hyperlordosis. In such cases, early diagnosis and intervention are crucial for managing symptoms and preventing complications.
Trauma and Medical Conditions
Injuries or trauma to the spine, such as fractures or disc herniation, can alter the natural curvature of the lumbar region. The body often compensates for these injuries by changing posture, which can lead to hyperlordosis or hypolordosis. Surgical interventions, if improperly rehabilitated, can also contribute to these postural changes.
Certain medical conditions, such as spondylolisthesis (slippage of a vertebra), osteoporosis, and ankylosing spondylitis, are associated with lumbar lordosis abnormalities. These conditions can weaken the structural integrity of the spine, leading to increased curvature or misalignment.
Managing trauma-related or medical causes of lumbar lordosis requires a multidisciplinary approach. Physical therapy, osteopathic treatments, and, in some cases, surgical intervention may be necessary to restore spinal health and alleviate symptoms.
Symptoms of lumbar hyperlordosis
The symptoms of lumbar hyperlordosis are diverse and may include pain in the lumbar region, accompanied by discomfort or pain in the hip area due to the anterior tilt of the pelvis. This condition can also influence posture, manifesting itself as an accentuated curvature and sometimes leading to muscle stiffness. Mobility may be reduced, and muscle fatigue may occur due to the constant effort required to maintain proper posture. In more severe cases, hyperlordosis can even lead to respiratory complications, highlighting the importance of early management and treatment of this condition. A consultation with a healthcare professional, such as an osteopath, is recommended for a thorough assessment and recommendations tailored to each specific case.
- Lower Back Pain: Pain in the lumbar region is one of the most common symptoms of hyperlordosis. This pain can be chronic and increase with physical activity.
- Discomfort: People with hyperlordosis may experience general discomfort in the lumbar region due to excessive curvature of the spine.
- Muscle Fatigue: Back muscles can fatigue more quickly due to increased tension caused by excessive lordosis.
- Limited Movements: Some individuals may have difficulty performing certain movements, such as bending forward, due to excessive curvature of the spine.
- Respiratory Problems: In severe cases of hyperlordosis, excessive curvature can affect the chest space, potentially lead to compression of internal organs, and cause breathing problems.
- Posture Alterations: Excessive lordosis can lead to noticeable changes in posture, such as a protruding buttocks or an accentuated curvature of the lower back.
- Neuralgia Sensations: In some cases, excessive lordosis can put pressure on the nerves in the spine, causing neuralgia sensations in the legs.
- Digestive Problems: In severe cases, hyperlordosis can affect the abdominal area, potentially leading to digestive problems.
Pathophysiology
Lumbar hyperlordosis is a condition characterized by excessive curvature of the lumbar region of the spine. Its pathophysiology involves a series of factors. Most of the time, it is linked to a muscular imbalance between the hip flexor muscles and the trunk extensor muscles.
Weakening of the abdominal muscles, combined with shortening of the hip flexors and lumbar muscles, can contribute to an anterior tilt of the pelvis, thereby accentuating the lumbar curvature. Postural imbalances and inappropriate movement habits can also play a crucial role.
Underlying causes of hyperlordosis include genetic factors, previous injuries, medical conditions such as spondylolisthesis, and sometimes neurological disorders. Pregnancy in women may also be associated with temporary hyperlordosis due to hormonal changes and weight redistribution.
- Abnormal Curvature: Hyperlordosis manifests as excessive curvature of the spine in an anterior (forward) direction. Under normal circumstances, the spine has natural curvatures that contribute to stability and mobility.
- Muscle Imbalance: An imbalance between the muscles of the back, abdominals and hips can contribute to hyperlordosis. Weak abdominal muscles combined with tight back muscles can lead to excessive pelvic tilt, contributing to increased lumbar curvature.
- Ligament Tension: The ligaments that support the spine can experience excessive strain due to increased curvature. This can lead to spinal instability and contribute to the progression of hyperlordosis.
- Modification of Natural Curvatures: Normal curvatures of the spine include lumbar lordosis and thoracic kyphosis (backwards curvature). Hyperlordosis can alter these natural curvatures, leading to abnormal posture.
- Genetic Factors: Some people may be genetically predisposed to developing excessive lordosis due to specific anatomical characteristics of their spine.
- Obesity: Excess weight, especially around the abdominal region, can shift the body’s center of gravity and contribute to increased lordosis.
- Pregnancy: During pregnancy, extra weight in the abdominal area can lead to increased lordosis in some women. Hormonal changes associated with pregnancy can also influence joint stability.
- Trauma or Injuries: Trauma, injuries, or previous surgeries can change the structure of the spine, contributing to hyperlordosis.
- Neurological Conditions: Certain neurological conditions, such as polio, muscular dystrophy, or other diseases affecting the muscles and nerves, may contribute to excessive lordosis.
Biomechanics
The muscle biomechanics of hyperlordosis involve changes in spinal alignment and changes in the forces exerted on muscle and joint structures. Here is a detailed explanation of the biomechanics associated with hyperlordosis:
- Psoas and Pelvic Tilt: Hyperlordosis is often associated with an anterior tilt of the pelvis. The psoas muscle, located in the lumbar region and attached to the femur, can play a key role in this shift. A tight psoas can pull the pelvis forward, contributing to excessive curvature of the lumbar spine.
- Piriformis and Pelvic Rotation: The piriformis, a deep muscle in the pelvic region, may also be involved. Its action on hip rotation can influence the position of the pelvis. Excessive rotation of the pelvis can worsen hyperlordosis.
- Change in Point of Gravity: Hyperlordosis shifts the body’s center of gravity forward. This can create increased load on the lower back muscles and joints of the spine, increasing stress on these structures.
- Formation of Dorsal Kyphosis: To compensate for the increased curvature in the lumbar region, some people with hyperlordosis develop dorsal kyphosis (backwards curvature) at the thoracic level. This helps maintain postural balance.
- Lumbar Facets and Premature Wear: The facet joints between the lumbar vertebrae may be subjected to uneven pressure due to hyperlordosis. This can lead to premature wear of joint surfaces, increasing the risk of degenerative spinal disorders.
- Disc Compression: Hyperlordosis can lead to compression of the intervertebral discs. Constant compression can contribute to disc degeneration and, in some cases, disc herniation.
- Nerve Root Compression: Advanced disc degeneration associated with hyperlordosis can compress the nerve roots emerging from the spine. This can lead to symptoms such as radicular pain, numbness, or weakness in the lower extremities.
- Discomfort in the Legs: Due to compression of the nerve roots, feelings of discomfort, pain or numbness may spread down the lower extremities.
Prevention of Lumbar Lordosis
Prevention of hyperlordosis is essential to maintaining optimal spinal health. Here are some tips and preventive practices:
- Maintaining Good Posture: Encourage patients to use correct posture when sitting, standing, and even walking. This includes maintaining the natural curvature of the spine.
- Muscle-strengthening exercises: Targeted exercises to strengthen the core muscles, particularly the abdominals and lower back muscles, can help stabilize the spine and prevent hyperlordosis.
- Regular stretching: Encourage regular stretching to maintain muscle and joint flexibility. This can help prevent stiffness and muscle imbalances.
- Weight Management: Maintaining a healthy body weight is crucial, as excess weight can put additional strain on the spine, contributing to the development of hyperlordosis.
- Ergonomics at work: Advise on the importance of good ergonomics at work to avoid prolonged sitting and encourage regular breaks to move.
Case studies :
Case study: Isabelle, 40 years old
Journey: Isabelle, a teacher in Quebec, consulted an osteopath due to persistent lower back pain and difficulty maintaining a comfortable posture in class.
Treatment methods: After a thorough assessment, the osteopath identified imbalances in Isabelle’s lumbar region, contributing to her hyperlordosis. The osteopathic-exclusive treatment plan included gentle mobilizations to restore spinal alignment, myofascial release techniques to release muscle tension, and advice on daily postural adjustments.
Results: Over the course of the osteopathy sessions, Isabelle felt a gradual improvement in her lower back pain. The manipulations and release techniques helped reduce pressure on his spine, improving his posture. Isabelle also learned specific exercises recommended by the osteopath to strengthen her muscles and maintain the gains obtained.
Isabelle’s story highlights osteopathy’s ability to successfully treat hyperlordosis using specific manual techniques and a personalized approach. The collaboration between the osteopath and the patient played a crucial role in obtaining positive results.
Osteopathic Approach to Lumbar Lordosis
Osteopathy views the body as an integrated whole, where structure and function are interdependent. This philosophy is particularly relevant when addressing lumbar lordosis, as the condition often involves compensatory changes in surrounding areas such as the pelvis, hips, and thoracic spine.
Key osteopathic principles include:
- Restoring balance in the musculoskeletal system.
- Improving mobility and alignment of the spine and pelvis.
- Enhancing the body’s natural healing capacity through non-invasive techniques.
The osteopathic approach involves a thorough assessment to determine the underlying causes of the abnormal curvature and how it impacts the patient’s overall biomechanics.
Techniques Used in Osteopathy for Lordosis
Osteopaths use a variety of hands-on techniques tailored to the patient’s specific condition. These include:
- Soft Tissue Techniques
These methods aim to release tension in tight muscles and fascia, particularly in the lower back, hip flexors, and hamstrings. For individuals with hyperlordosis, relaxing the psoas muscle—a key contributor to anterior pelvic tilt—can significantly reduce excessive curvature. - Myofascial Release
By addressing fascial restrictions, osteopaths help restore flexibility and mobility. Myofascial release is especially effective in patients with chronic muscle tightness or postural imbalances contributing to lordosis. - Spinal Mobilization and Manipulation
Gentle mobilizations improve joint range of motion and alleviate discomfort. In cases of lumbar lordosis, manipulation of the lumbar and sacral regions can help restore proper alignment and reduce compensatory strain in other areas. - Postural Re-education
Osteopaths guide patients in identifying and correcting poor postural habits. This may involve exercises to strengthen core muscles, improve pelvic alignment, and support the natural curve of the lumbar spine. - Cranial Osteopathy
Although less directly related to the lumbar region, cranial techniques can support the overall balance of the nervous system and promote relaxation, indirectly benefiting posture and muscle tone.
Lordosis and the Fetal Position in Adults
The fetal position, characterized by the flexion of the spine, hips, and knees, is often adopted instinctively for comfort and relief from spinal strain. For individuals with hyperlordosis, adopting a fetal position can temporarily alleviate tension in the lower back by reducing the excessive lumbar curve. Osteopaths may use this insight to recommend stretches or exercises that mimic the fetal position, such as child’s pose in yoga, to provide relief and promote spinal flexibility.
Conversely, in individuals with hypolordosis, the osteopathic approach may emphasize opening the spine and encouraging the restoration of the natural curve. Techniques to strengthen the lower back extensors and improve pelvic tilt are often combined with gentle mobilizations.
Addressing the Root Causes
An osteopath takes a comprehensive approach to identifying and addressing the root causes of lumbar lordosis. Common contributors include:
- Postural Imbalances: Correcting forward pelvic tilt and strengthening the core.
- Muscle Weakness or Tightness: Stretching tight hip flexors and strengthening abdominal muscles.
- Lifestyle Factors: Ergonomic assessments and lifestyle modifications to reduce strain on the lower back.
- Developmental Factors: Identifying and addressing any motor development issues that may have impacted spinal alignment during growth.
Conclusion
Self-management tips
- Abdominal strengthening exercises: Regularly practice exercises targeting the abdominal muscles, such as crunches and planks, to strengthen the core region and stabilize the spine.
- Lower back muscle stretches: Incorporate specific stretches for the lower back muscles, such as psoas muscle stretches, to promote flexibility and relieve tension.
- Strengthening the back muscles: Include strengthening exercises for the back muscles, such as back extensions, to balance muscle strength between the front and back of the trunk.
- Maintaining a good sitting posture: Adopt a correct sitting posture by maintaining the natural curvature of the spine. Use a lumbar cushion if necessary to support the lumbar region.
- Break and Stretch at Work: Take regular breaks at work to stand, stretch, and change positions. This helps prevent muscle fatigue and improve circulation.
- Using lumbar support: If you spend a lot of time sitting, use appropriate lumbar support on your chair to maintain the natural curvature of the spine.
- Maintaining a healthy body weight: Adopt a healthy lifestyle with a balanced diet and regular exercise to maintain an optimal body weight, thereby reducing pressure on the spine.
- Postural education: Learn about good postural practices in different daily activities, such as lifting objects, to avoid excessive pressure on the spine.
- Relaxation exercises: Practice relaxation exercises, such as meditation or deep breathing, to reduce stress and muscle tension.
- Regular consultations with a healthcare professional: Schedule regular consultations with an osteopath to assess your posture and receive personalized advice on managing hyperlordosis.
Stretches and exercises
Stretching
- Stretching the psoas muscle:
- Get on your knees on the floor.
- Step one leg forward while keeping the other bent behind you.
- Tilt your pelvis slightly forward until you feel a stretch in your hip area.
- Hip flexor stretch:
- Sit on the floor with your legs extended.
- Bend one leg and place the foot on the inner thigh of the other leg.
- Lean your upper body slightly forward, keeping your back straight.
- Étirement du quadratus lumborum :
- Sit in a chair with your back straight.
- Lean slightly to one side, bringing the ear towards the shoulder, to stretch the muscles on the side of the spine.
Strengthening exercises
- Plank :
- Assume a push-up position with your arms straight.
- Maintain the position by contracting your abdominal muscles and keeping your back straight. Start with short intervals and gradually increase the duration.
- Extensions two:
- Lie face down on the floor.
- Gently lift your chest off the floor using your lower back muscles. Hold the position for a few seconds.
- Lying leg raises:
- Lie on your back with your arms at your sides.
- Raise both legs toward the ceiling, contracting your abdominal muscles, then slowly lower back down.
- Reverse crunches:
- Lie on your back with your legs bent at 90 degrees.
- Lift your lower back off the floor by contracting your abs, bringing your knees closer to your chest.
- Candle exercise (against a wall):
- Lie on your back with your buttocks against the wall.
- Raise your legs along the wall, keeping your lower back flat on the floor. This strengthens the abdominal and back muscles.
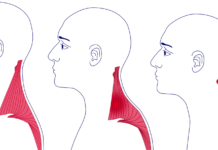
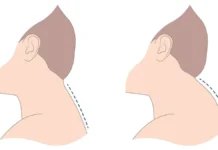
Postural assessment
- Slight plantar flexion of the ankle possible.
- Slight hyperextension of the knee possible.
- Hip flexion
- Bilateral anterior pelvic tilt in hyperlordosis is greater than 10 degrees in women and greater than 5 degrees in men.
- Lumbar lordotic curve is increased.
- Compensatory hyperkyphosis
- Forward head posture.

Questionnaire 1
- What is hyperlordosis and how is it characterized?
- a) An accentuated curvature of the cervical region
- b) An accentuated curvature of the thoracic region
- c) An accentuated curvature of the lumbar region
- d) An accentuated curvature of the sacral region
- How important is lumbar lordosis in human evolution?
- a) She did not play a significant role
- b) It contributed to human bipedalism
- c) It caused posture problems
- d) It caused lower back pain
- How did lumbar lordosis benefit our ancestors?
- a) By making walking difficult
- b) By absorbing shocks while walking
- c) By limiting trunk mobility
- d) By causing respiratory problems
- What modern factors can contribute to hyperlordosis?
- a) A natural bipedal posture
- b) An increase in physical activity
- c) A sedentary lifestyle and being overweight
- d) Adaptation to natural conditions
- What are the possible causes of hyperlordosis?
- a) Correct posture
- b) Strong abdominal muscles
- c) Genetic conditions, trauma, and muscular imbalances
- d) Regular physical activity
Symptoms and Pathophysiology
- What are the common symptoms of lumbar hyperlordosis?
- a) Pain in the cervical region
- b) Pain in the shoulders
- c) Pain in the lumbar region, discomfort, muscle fatigue, alterations in posture
- d) Abdominal pain
- What primarily contributes to anterior pelvic tilt in hyperlordosis?
- a) Weakening of the back muscles
- b) Contracture du muscle psoas
- c) Atrophy of the abdominal muscles
- d) Stiffness of the muscles of the lower limbs
- How can hyperlordosis affect the intervertebral discs?
- a) By strengthening them
- b) By compressing them, contributing to degeneration
- c) By isolating them from the rest of the spine
- d) By making them more flexible
Prevention and Self-management Tips
- What tips are recommended for the prevention of hyperlordosis?
- a) Maintaining poor posture
- b) Avoidance of stretching
- c) Weight management, muscle strengthening exercises, and maintaining good posture
- d) Ignoring early signs
Case Study and Conclusion
- What treatment method was used successfully in Isabelle’s case study?
- a) Surgery
- b) Medication
- c) Exclusive approach to osteopathy
- d) No treatment was applied
Answers:
- c) An accentuated curvature of the lumbar region
- b) It contributed to human bipedalism
- b) By absorbing shocks while walking
- c) A sedentary lifestyle and being overweight
- c) Genetic conditions, trauma, and muscular imbalances
- c) Pain in the lumbar region, discomfort, muscle fatigue, alterations in posture
- b) Contracture du muscle psoas
- b) By compressing them, contributing to degeneration
- c) Weight management, muscle strengthening exercises, and maintaining good posture
- c) Exclusive approach to osteopathy
Conclusion
Lumbar lordosis, a natural inward curve of the lower spine, is essential for balance, flexibility, and shock absorption. However, deviations from the normal curvature, whether excessive (hyperlordosis) or reduced (hypolordosis), can lead to discomfort, postural challenges, and even significant health complications if left unaddressed. Understanding its causes, symptoms, and treatments is critical for maintaining spinal health and overall well-being.
Recap of Key Points
We explored the primary causes of lumbar lordosis, including poor posture, obesity, pregnancy, muscle imbalances, neurological factors, and trauma or medical conditions. Each of these factors can alter the natural alignment of the spine, leading to changes that affect mobility and quality of life.
Poor posture, often stemming from sedentary lifestyles and prolonged sitting, is a leading cause. Muscle imbalances, such as weak abdominal muscles or tight lower back muscles, exacerbate the issue. Obesity and pregnancy contribute to additional strain on the spine, while neurological conditions and trauma can further disrupt spinal alignment.
Prevention and self-care are crucial in addressing these issues. Practicing good posture, engaging in targeted exercises, and maintaining a healthy weight can significantly reduce the risk of developing abnormal spinal curvature. For more complex cases, however, professional intervention is essential.
Importance of Professional Care
While many self-care strategies can alleviate mild symptoms and prevent further complications, professional care remains indispensable for effectively diagnosing and treating lumbar lordosis. Healthcare professionals, such as osteopaths, physical therapists, and orthopedic specialists, bring expertise and tailored approaches to managing spinal health.
Osteopathic care, in particular, emphasizes holistic treatment, focusing on restoring balance and mobility to the musculoskeletal system. Techniques such as myofascial release, spinal manipulation, and postural training can address the underlying causes of lumbar lordosis and relieve associated discomfort.
Early consultation with a professional is critical, especially if symptoms like persistent lower back pain, limited mobility, or postural changes occur. Ignoring these signs can lead to worsening conditions, including nerve compression, disc degeneration, and chronic pain. A thorough evaluation by a healthcare provider ensures accurate diagnosis and a personalized treatment plan.
Final Thoughts
Lumbar lordosis is a dynamic aspect of spinal anatomy, vital to our posture and movement. However, when imbalances occur, it is essential to address them promptly through a combination of self-care and professional support. By understanding its causes, symptoms, and treatment options, individuals can take proactive steps toward maintaining a healthy spine and improving their overall quality of life. Prioritizing professional care ensures the best outcomes for long-term spinal health and well-being.
References
- Been E, Kalichman L. Lumbar lordosis. Spine J. 2014; 14(1): 87–97. 10.1016/j.spinee.2013.07.464 [PubMed] [CrossRef] [Google Scholar]
- Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am . 2005; 87: 260–267. [ PubMed ] [ Google Scholar
- Vrtovec T, Likar B, Pernus F. Quantitative analysis of spinal curvature in 3D: Application to CT images of normal spine. Phys Med Biol. 2008; 53: 1895–1908. 10.1088/0031-9155/53/7/006 [PubMed] [CrossRef] [Google Scholar]
- Cobb J. Outline for the study of scoliosis. Amer Acad Orthop Surg Instructional Course Lectures. 1948; 5:261–275. [Google Scholar]
- Harrison DE, Harrison DD, Cailliet R, Janik T, Holland B. Radiographic analysis of lumbar lordosis: Centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine. 2001; 26: E235–E242. [PubMed] [Google Scholar]
- Voutsinas S, MacEwen G. Sagittal profiles of the spine. Clin Orthopaed Related Res. 1986; 210: 235–242. [PubMed] [Google Scholar]
- Hicks G, George S, Nevitt M, Cauley J, Vogt M. Measurement of lumbar lordosis: Inter-rater reliability, minimum detectable change and longitudinal variation. J Spinal Disord. 2006; 19: 501–506. [PubMed] [Google Scholar]
- Polly D, Kilkelly F, McHale K, Asplund L, Mulligan M, Chang A. Measurement of lumbar lordosis: Evaluation of intraobserver, interobserver, and technique variability. Spine. 1996; 21:1530–1535. [PubMed] [Google Scholar]
- Norton BJ, Sahrmann SA, Van Dillen LR. Differences in measurements of lumbar curvature related to gender and low back pain. J Orthopaed Sports Phys Therapy. 2004; 34: 524–534. [PubMed] [Google Scholar]
- Korovessis PG, Stamatakis MV, Baikousis AG. Reciprocal angulation of vertebral bodies in the sagittal plane in an asymptomatic Greek population Spine. 1998; 23: 700–704. [PubMed] [Google Scholar]
- Janssen MM, Drevelle X, Humbert L, Skalli W, Castelein RM. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine. 2009; 34: E826–E832. 10.1097/BRS.0b013e3181a9fd85 [PubMed] [CrossRef] [Google Scholar]
- Kim H, Kim HS, Moon ES, Yoon CS, Chung TS, Song HT, et al. Scoliosis imaging: what radiologists should know. Radiographics. 2010; 30: 1823–42. 10.1148/rg.307105061 [PubMed] [CrossRef] [Google Scholar]
- Rangayyan RM, Deglint HJ, Boag GS. Method for the automatic detection and segmentation of the spinal canal in CT images. J Electron Imaging. 2006; 15: 033007 10.1117/1.2234770 [CrossRef] [Google Scholar]
- Klinder T, Ostermann J, Ehm M, Franz A, Kneser R, Lorenz C. Automated model-based vertebra detection, identification, and segmentation in CT images. Med Image Anal. 2009; 13: 471–482. 10.1016/j.media.2009.02.004 [PubMed] [CrossRef] [Google Scholar]
- McInerney T, Terzopoulos D. Deformable models in medical image analysis: A survey. Med Image Anal. 1996; 1: 91–108. [PubMed] [Google Scholar]
- Andrews J, Sethian J. Fast marching methods for the continuous traveling salesman problem. Proc Nat Acad Sci 2007; 104: 1118–1123. [PMC free article] [PubMed] [Google Scholar]
- Perneger TV. What is wrong with Bonferroni adjustments. Br Med J. 1998; 136: 1236–1238. [PMC free article] [PubMed] [Google Scholar]
- Sankoh AJ, Huque MF, Dubey SD. Some comments on frequently used multiple endpoint adjustments methods in clinical trials. Stat Med. 1997; 16: 2529–2542. [PubMed] [Google Scholar]