Hand osteoarthritis is a degenerative disease of the hand joints characterized by the deterioration of cartilage, leading to pain, stiffness, and loss of function.
Introduction – When Hands Freeze: Understanding Digital Osteoarthritis
Our hands tell our story. They create, heal, communicate, and accompany. They translate our most subtle thoughts, our deepest emotions, and our most spontaneous impulses into gestures. Every day, they perform hundreds of movements, often without our awareness. Yet, for many people, these movements become a source of pain, stiffness, and frustration. Osteoarthritis of the hand, insidious and progressive, transforms the natural expression of gesture into a struggle against blockage, deformation, and discomfort.
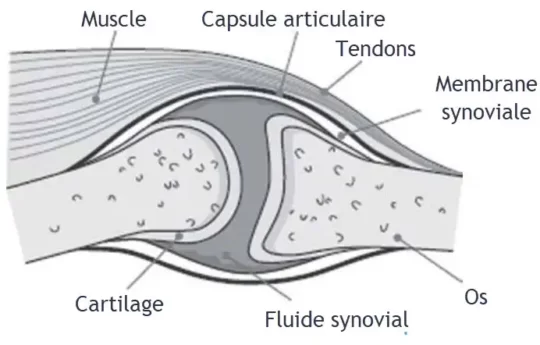
Osteoarthritis is a degenerative joint disease that particularly affects older people, but it does not spare younger people, especially when genetic, hormonal, or traumatic factors are involved. It manifests itself through a progressive deterioration of cartilage, the soft, smooth tissue that covers the ends of bones within joints. When this cartilage diminishes or disappears, the bones rub directly against each other, causing pain, inflammation, and the formation of bony growths called osteophytes.
Hand osteoarthritis affects several anatomical regions: the distal interphalangeal (DI) joints at the fingertips, the proximal interphalangeal (PI) joints in the center of the fingers, and the carpometacarpal (CMC) joints, particularly those of the thumb. It is one of the most common forms of osteoarthritis, particularly in postmenopausal women. Although often considered a “natural” consequence of aging, it represents a real public health issue due to its functional and emotional impact.
Because living with hand osteoarthritis isn’t just about pain. It can also mean having to give up simple tasks: buttoning a shirt, peeling vegetables, writing, playing an instrument, or simply holding a loved one’s hand. These limitations can compromise autonomy, identity, and quality of life. Additionally, visible finger deformities—often associated with the formation of Bouchard and Heberden nodules—can affect body image and self-image.
The complexity of osteoarthritis also lies in its variability. Some individuals live with advanced radiographic lesions but little pain, while others suffer intensely with few visible signs. This discordance between structure and sensation shows that osteoarthritis is not simply a mechanical disease. It is part of a broader context, where biological, hormonal, emotional, and environmental factors interact.
Currently, there is no curative treatment for osteoarthritis. Treatment therefore aims to relieve symptoms, maintain mobility, and improve quality of life. While conventional medicine offers anti-inflammatory drugs, injections, or sometimes surgery, other approaches—such as osteopathy—seek to support the individual as a whole, restoring movement to tissues, reducing mechanical stress, and promoting the body’s self-regulation.
This article offers a comprehensive exploration of hand osteoarthritis: its forms, causes, clinical manifestations, consequences, as well as available therapeutic strategies, including the osteopathic approach. We will see that, even if this condition is chronic, it is possible to act on several levels to reduce pain, slow its progression, and regain a certain freedom of movement.
Through this journey, we also hope to restore a place to these hands, often forgotten, injured, or aged too quickly, but which remain at the heart of our humanity. Because they touch, shape, embrace, and express… our hands deserve to be listened to, understood, and cared for.
Common symptoms and clinical signs of hand osteoarthritis
Hand osteoarthritis manifests gradually, often insidiously. In its early stages, it may go unnoticed or be mistaken for simple joint fatigue. However, as cartilage degradation progresses, the signs become more evident, affecting not only movement but also the very structure of the joints. Understanding the typical symptoms of this condition is essential for early diagnosis, slowing its progression, and providing appropriate treatment.
Joint pain: a common initial complaint
Pain is the most common symptom. It usually occurs during exercise , when the hand is used for everyday tasks: turning a key, cutting food, writing, opening a jar. This pain can also appear after activity , or at the end of the day, indicating a state of chronic inflammation of the joint. It is often described as dull, deep , and difficult to locate precisely .
As the disease progresses, the pain may become more persistent , occurring even at rest or at night, and disrupting sleep. Some people report episodes of acute pain, particularly during inflammatory flare-ups in erosive forms.
Morning or post-inactivity stiffness
Another telltale sign is joint stiffness , often observed in the morning upon waking or after a prolonged period of inactivity (reading, driving, resting). This stiffness, which is transient, generally lasts less than 30 minutes , which helps differentiate it from inflammatory forms such as rheumatoid arthritis, where stiffness can last more than an hour.
Over time, this stiffness can worsen, and fine movements become more difficult to initiate, making it difficult to open the hand or fully flex the fingers.
Joint swelling: subtle but persistent inflammation
In the active phases of osteoarthritis, localized swelling is often observed in the interphalangeal joints. It is usually not red and not very warm , which distinguishes it from more acute inflammatory conditions. This swelling is due to a combination of synovial irritation, capsular thickening and, sometimes, the presence of bone nodules (osteophytes).
It may be accompanied by painful stretching of the joint capsule , making certain positions uncomfortable, particularly prolonged gripping of an object.
Joint crackling or popping sounds
When cartilage deteriorates, bone surfaces become uneven, resulting in cracking or rubbing sounds during movement. This phenomenon, called crepitus , is common in the interphalangeal and carpometacarpal joints. Although these sounds are not always painful, they indicate a loss of joint congruity and may be uncomfortable for the patient due to their unusual nature.
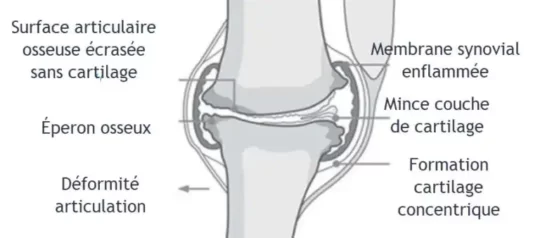
Joint deformities and characteristic nodules
At a more advanced stage, hand osteoarthritis leads to visible changes in joint morphology. The two most characteristic deformities are:
- Bouchard nodules , located on the proximal interphalangeal (IP) joints.
- Heberden’s nodes , located on the distal interphalangeal (DI) joints.
These bony growths are often bilateral and symmetrical. They are evidence of ossification secondary to repeated microtraumas and the uncontrolled repair of destroyed cartilage. In addition to their aesthetic impact, they can limit joint range of motion and cause discomfort during fine movements.
Loss of strength and mobility
As the disease progresses, there is a progressive reduction in grip strength , particularly in tasks requiring thumb-index finger opposition (holding a pen, buttoning a garment). Finger mobility is also compromised: some joints become rigid, others compensate by developing secondary hyperlaxity, creating imbalances in the muscle chains of the hand.
This functional loss directly impacts autonomy and quality of life , by limiting the performance of everyday actions.
Sensitivity to touch and allodynia
Some arthritic joints become sensitive to simple contact , even without movement. This hypersensitivity is linked to chronic irritation of joint receptors, sometimes accompanied by capsular edema . It can lead to a spontaneous reduction in the use of the hand , promoting ankylosis and muscle wasting.
Evolution by thrusts and stabilization phases
Hand osteoarthritis does not always progress in a linear fashion. It can alternate between phases of painful flare-ups (inflammation, swelling, increased stiffness) and phases of partial remission , where pain decreases and function improves. This intermittent progression is typical of erosive forms and must be well understood in order to adapt treatments.
The different forms of hand osteoarthritis
Hand osteoarthritis is not a homogeneous entity. It manifests itself in several distinct forms, depending on the joints involved, the speed of progression, the inflammatory context or not, and the radiographic characteristics. A good understanding of these variants is essential to make a differential diagnosis, adapt therapeutic management, and anticipate functional evolution. Among the most frequent forms, we distinguish: nodular osteoarthritis , erosive osteoarthritis , and osteoarthritis of the carpometacarpal (CMC) joint of the thumb .
Nodular osteoarthritis: the most visible form
Nodular osteoarthritis is probably the most classic and recognizable form of digital osteoarthritis. It mainly affects the distal interphalangeal (DI) and proximal interphalangeal (PI) joints , i.e. the tips and center of the fingers.
This form is characterized by the appearance of bone nodules , called respectively:
- Heberden nodules at the distal joints
- Bouchard nodules at the proximal joints
These bony growths are the result of bone remodeling secondary to the degradation of articular cartilage. They often appear bilaterally and symmetrically, particularly in postmenopausal women, and may be accompanied by stiffness, pain on pressure or movement, and visible deformities.
The progression is generally slow and progressive , interspersed with phases of moderate inflammatory flare-ups. The pain sometimes subsides once the nodules have stabilized, but functional discomfort may persist, particularly during fine or prolonged movements.
Radiologically , we observe:
- Joint space reduction
- Marginal osteophytes
- Subchondral sclerosis
- Structural deformations
This form of osteoarthritis, although often well tolerated systemically, can profoundly alter the patient’s dexterity and body image.
Erosive osteoarthritis: a more aggressive and inflammatory form
Erosive osteoarthritis is a rarer but significantly more painful and destructive variant . It mainly affects the proximal interphalangeal (IP) joints , but can also affect other small digital joints.
It is characterized by a marked inflammatory process that is accompanied by rapid destruction of the cartilage and underlying bone , hence the term “erosive”. Symptoms are often more sudden, severe , with phases of acute pain, significant swelling, local redness and a sensation of heat, sometimes confused with an inflammatory pathology such as rheumatoid arthritis.
Joints become sensitive, unstable, and rapidly deform, with significant functional loss. In some cases, joint ankylosis (permanent locking) can occur if the disease is not treated early.
On the radiological level , we find:
- Central or marginal erosions
- Disappearance of the joint space
- Irregular osteophytes
- Asymmetrical damage in some cases
This form of osteoarthritis often requires a multidisciplinary approach, with careful medical monitoring, functional adaptation, and osteopathic care that respects the acute inflammatory state.
CMC osteoarthritis of the thumb: a major functional challenge
The carpometacarpal (CMC) joint of the thumb, located at the base of the thumb, is particularly vulnerable to osteoarthritis. It is a saddle joint, extremely mobile, but subject to significant mechanical stress , particularly during pinching, rotation and gripping movements.
CMC osteoarthritis of the thumb affects more women after the age of 50, and its development can be favored by a history of trauma or ligament hyperlaxity.
Typical symptoms:
- Pain at the base of the thumb, especially when gripping objects
- Decrease in pinch force (between thumb and index finger)
- Visible deformity (subluxation, widening of the base)
- Stiffness and instability
Pain is often felt at the end of the day , during repetitive or rotating movements (opening a jar, turning a key).
Diagnosis is based on clinical examination (Grind test, axial compression test of the thumb) and X-ray, which reveals narrowing of the joint space , osteophytes , and sometimes dorsal subluxation of the first metacarpal.
Treatment is based on a combination of measures: joint rest, stabilization orthosis, functional rehabilitation, osteopathy, infiltrations, and even surgery in severe cases.
Typical nodules: Bouchard and Heberden
Among the most suggestive clinical signs of hand osteoarthritis, Bouchard and Heberden nodes hold a central place. These visible and palpable bony growths are the result of chronic joint remodeling, a sign of the wear and tear and uncontrolled repair of cartilage. They are not simply aesthetic: they reflect prolonged joint pain, affect hand function, and can cause pain, stiffness, and coordination problems.
Origin and mechanism of formation
When the cartilage covering the ends of bones thins or disappears—as occurs in osteoarthritis—the bones rub against each other, causing inflammation, microtrauma, and instability. In response, the body attempts to “repair” the joint structure by stimulating bone growth. This process of new formation, although intentional, results in bony growths called osteophytes that accumulate around the joint, gradually forming nodules.
These nodules can appear without pain or, on the contrary, be preceded by acute inflammatory phases , with pain, redness and functional limitation. Once stabilized, they often become painless but leave lasting mechanical after-effects.
Heberden’s Nodes
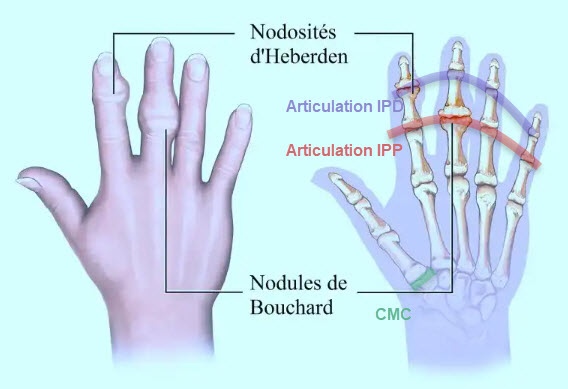
Heberden’s nodes are located at the distal interphalangeal (DI) joints , the joints closest to the fingertips.
Clinical features:
- Location : Fingertips, just before the nail.
- Appearance : Small, hard growths visible on the top (dorsal) of the joints.
- Symmetry : Often present on both sides, although their appearance may be gradual.
- Pain : They may be sensitive to pressure, especially early in their formation.
- Mobility : discomfort with flexion/extension may occur, impairing fine movements.
Historical context:
These nodules are named after William Heberden (1710–1801), a British physician who was one of the first to describe them. He noted their prevalence in older women and their often hereditary nature. Even today, their presence is an important diagnostic criterion in digital osteoarthritis.
Bouchard’s nodules
Less well known to the general public but just as significant, Bouchard nodules appear at the proximal interphalangeal (IP) joints , located in the center of the fingers.
Clinical features:
- Location : intermediate joint, between the proximal and middle phalanges.
- Appearance : firm nodules, sometimes less visible than those of Heberden but just as limiting.
- Sensitivity : often painful to pressure and movement, especially during arthritic flare-ups.
- Function : they limit the complete flexion of the finger, disrupting everyday gestures (gripping objects, writing, fine manipulation).

Historical context:

These nodules are named after the French physician Charles-Joseph Bouchard (1837–1915), a pioneer in the understanding of degenerative joint diseases. He highlighted their link with chronic inflammatory processes and structural damage visible on radiology.
Functional and aesthetic consequences
Bouchard and Heberden nodules are not just “bumps.” Their appearance is accompanied by profound joint changes :
- Reduced range of motion
- Change in the axis of the fingers (deviation or angulation)
- Discomfort during fine movements: writing, fastening a button, pinching
- Aesthetic and psychological impact, especially in young or very active patients
Some people also develop a compensatory attitude, putting more strain on the unaffected joints, which can in turn promote wear and tear
Differential diagnosis and imaging
Radiographically, these nodules are generally accompanied by:
- Joint space narrowing
- Osteophytes clearly visible
- Subchondral sclerosis
- Deformation of the bone head
It is important to differentiate them from arthritic nodules (rheumatoid arthritis), tophi (gout), or other causes of digital swelling. The hard, progressive, bilateral nature associated with degenerative radiographic signs is suggestive of osteoarthritis.
Few curative treatments, but support options
No therapy can “make nodules disappear.” However, several approaches can relieve pain, maintain mobility, and slow progression :
- Psychosomatic approach , to explore the relationship to loss of function and body image
- Resting or functional orthoses
- Gentle mobilizations in osteopathy to reduce periarticular tension
- Paraffin baths, hot compresses, flexibility exercises
- Anti-inflammatory diet , rich in omega-3 and antioxidants
Causes and risk factors of hand osteoarthritis
Hand osteoarthritis is not a disease that occurs by chance. It results from a tangle of factors : natural aging, heredity, overuse, joint trauma, hormonal imbalances, mechanical overload, etc. Understanding the underlying causes and risk factors allows us to consider not only more targeted prevention, but also more comprehensive care, taking into account each person’s experience, environment, and constitutional background.
Joint aging: programmed wear and tear?
The most frequently cited factor remains age . Over time, cartilage thins , loses its ability to regenerate, and becomes more vulnerable to everyday microtraumas. This phenomenon is accentuated by a decrease in the cartilage’s hydration capacity, a lower production of synovial fluid, and an alteration of local cellular nutrition. This “wear and tear” is not universal, however: some older people will never develop significant osteoarthritis, while others will see their hands become deformed from the age of fifty.
The role of genetics: silent inheritance
Numerous studies have highlighted a genetic predisposition to hand osteoarthritis, particularly its nodular form. Heberden and Bouchard nodes frequently appear in several members of the same family, often spanning several generations. This susceptibility appears to be more pronounced in women. Certain genes related to collagen structure, cartilage metabolism, or inflammation regulation may play a determining role.
Thus, a patient can suffer from osteoarthritis without having had an accident or intense manual work, simply because her family background predisposes her to increased cartilage fragility.
Sex and hormonal influence
Hand osteoarthritis is significantly more common in women , especially after menopause. This is partly due to the decline in estrogen, a hormone known for its protective effects on joint tissue. Hormonal changes affect not only cartilage metabolism, but also pain perception, ligament laxity, and bone strength.
It is not uncommon to see digital osteoarthritis appear quickly after menopause, with marked inflammatory flare-ups, as in erosive osteoarthritis.
Repetitive trauma and microtrauma
Old trauma , even minor, can promote long-term joint degeneration. A fracture, a poorly healed sprain, old surgery or a direct shock can alter the biomechanics of a joint and accelerate cartilage wear.
Furthermore, repetitive movements or intensive manual activities (secretarial work, sewing, healthcare, music, gardening, mechanics, etc.) subject the hands to constant stress. This chronic joint stress can, over time, lead to micro-deterioration of the structures and trigger a degenerative cascade.
Obesity: an unknown influence on the hands
Obesity is often associated with osteoarthritis of the knees or hips, but it also plays a role in digital osteoarthritis. Not because of the mechanical load (the hands do not bear the body weight), but because of the systemic inflammatory effect of adipose tissue . The latter produces pro-inflammatory cytokines (such as leptin or TNF-alpha) that alter the quality of the cartilage remotely.
Thus, being overweight is an indirect but real risk factor for hand osteoarthritis.
Mechanical and postural anomalies
Chronic poor posture, joint axis disorders (deviated fingers, congenital hyperlaxity, ligament instability) or even impaired motor coordination can increase the stress on certain joints and accelerate their degeneration.
These imbalances, often discreet, can sometimes be corrected with osteopathy or occupational therapy if detected early.
Inflammatory joint diseases
Although osteoarthritis is not strictly an inflammatory disease, it can coexist with or be promoted by pathologies such as rheumatoid arthritis, lupus erythematosus or joint psoriasis . These chronic inflammatory conditions alter the structure of the joints, modify the composition of the cartilage and weaken the joint surfaces, creating a breeding ground for secondary osteoarthritis.
Metabolic and nutritional factors
Imbalances such as diabetes , hyperuricemia , or vitamin D and calcium deficiencies can influence joint health. The quality of cartilage tissue depends on many micronutrients, bone vascularization and the regulation of local metabolism.
Hand osteoarthritis in everyday life: functional impact and quality of life
Hand osteoarthritis is not limited to simple joint degeneration visible on an X-ray. It infiltrates the most basic, most familiar gestures, to the point of altering daily life in its most intimate dimensions. As joints become deformed, pain sets in, and mobility is reduced, the relationship with oneself, with others, with work, and with daily activities is disrupted. Osteoarthritis then becomes a lived experience, bodily, emotional, sometimes invisible but deeply felt.
The hand, a tool of daily life
Hands are at the heart of almost all of our interactions with the world: they dress, cook, write, touch, hold, caress, and communicate. When these functions are impaired, autonomy gradually crumbles. Simple gestures become restrictive, sometimes impossible:
- Fasten a bra, button a shirt
- Turn a key in a lock
- Open a jar or bottle
- Comb your hair, brush your teeth, put on a pair of gloves
- Write or use a telephone
These limitations affect not only domestic activities, but also professional or creative activities : gardening, music, crafts, sewing, office work, or caregiving. Some patients report a loss of efficiency, increased slowness, or the need to adapt their way of doing things. Others end up abandoning tasks or delegating, which can lead to feelings of frustration or helplessness.
Pain and fatigue: a constant effort to compensate
Chronic pain, even moderate pain, is exhausting over time. It is associated with secondary muscle contractions, constant bodily alertness, and generalized functional fatigue. Hand osteoarthritis not only hinders movement: it imposes a constant mental burden .
Additionally, painful discomfort sometimes forces us to compensate with other fingers, the palm, or even the forearm, which can create secondary tension in the elbow, shoulder, or even neck . The entire body adapts to protect a painful joint—at the risk of unbalancing other functional chains.
Impairment of grip and fine movements
One of the most specific impacts of hand osteoarthritis is the reduction in gestural precision , particularly in the thumb-index pinch, flexion of the distal phalanges, and joint stability. This alteration affects:
- Grasping small objects (coins, buttons)
- Fine rotational movements (key, pen)
- Prolonged presses (holding a book, a tablet)
- Force control (lifting a cup, squeezing a tube)
When joints lose their fluidity, confidence in the hand diminishes. Some patients avoid certain movements for fear of dropping an object or triggering pain.
Aesthetic impact and body image
The appearance of nodules (Heberden, Bouchard), visible deformations, and sometimes asymmetrical swelling of the fingers alter the patient’s image of their hand . This physical transformation is sometimes difficult to experience, particularly in women, or in people for whom hands are part of their identity (artists, therapists, teachers, artisans).
A deformed hand can become a source of social embarrassment, silent withdrawal, and even shame. Some patients hide their hands, avoiding gestures of affection or looking at their fingers.
Emotional and psychological repercussions
Hand osteoarthritis is often accompanied by a feeling of wear and tear , loss, and premature aging. In active people, it can cause anger, a sense of injustice, or anxiety about their professional future. In older people, it is sometimes experienced as a symbol of decline , a painful reminder of the body giving way.
Some studies show a link between painful osteoarthritis and mild to moderate depressive symptoms , particularly in older women living alone. Others highlight the burden of feelings of worthlessness , when a person can no longer perform the actions that made them feel useful or valued.
Adaptation and resilience: resources that can be mobilized
Despite these difficulties, many people develop remarkable coping strategies :
- Use of ergonomic accessories (jar openers, thickened pens)
- Learning new ways of doing things
- Benevolent delegation to those around you
- Gradual acceptance of certain renunciations
- Gentle body practices: osteopathy, yoga, paraffin baths, self-massages
Therapeutic support – whether osteopathic, occupational therapy or psychocorporeal – can play a key role in rebuilding the relationship with the hand , in revaluing its residual capacities , and in restoring the feeling of acting.
Diagnosis and additional examinations for hand osteoarthritis
Diagnosing hand osteoarthritis relies primarily on rigorous clinical observation , attentive listening to the patient and, when necessary, the support of medical imaging. While the symptoms are often suggestive, a precise diagnosis—making it possible to distinguish between different forms of osteoarthritis or rule out other pathologies—requires a cross-functional and morphological assessment. This approach is all the more essential since some patients present with diffuse or atypical pain, without visible deformity.
Anamnesis: listening to the speaking hand
The first step is to collect a detailed medical history . It is important to know:
- Location of pain (thumb, fingers, entire hand )
- The mode of appearance : sudden or gradual, post-traumatic or spontaneous
- Triggering factors : repetitive movements, carrying loads, exposure to cold
- The timing of the pain : early morning, late afternoon, nighttime?
- The presence of stiffness , swelling or cracking
- Functional impact : loss of strength, impossible movements, fatigue on exertion
- The existence of a family history of osteoarthritis
- Possible comorbidities : diabetes, obesity, hormonal disorders, inflammatory pathologies
This precise collection points towards classic, erosive osteoarthritis, or towards another joint pathology, such as inflammatory arthritis or a systemic pathology.
Clinical examination: observe, palpate, test
The clinical examination makes it possible to objectify the signs reported by the patient:
- Inspection : search for nodules (Heberden, Bouchard), deformations, swellings, redness, muscle atrophy
- Palpation : look for pain when pressing on the joints, local heat, crepitation
- Active and passive mobility : measurement of joint range of motion (flexion, extension, opposition of the thumb)
- Grip strength : hand squeeze test, thumb-index pinch, object lifting
- Specific tests :
- Grind test for the CMC joint of the thumb (rotation + painful compression)
- Ligament mobility test to exclude underlying instability
The observation of reduced mobility associated with mechanical pain (related to movement, relieved by rest) is typical of advanced osteoarthritis.
Standard X-rays: the reference examination
X-rays remain the key examination for confirming the diagnosis of osteoarthritis. They allow for direct visualization of bone structures and assessment of the stage of the disease.
The shots are generally taken from the front and from the side , in the functional position of the hand.
Typical radiological signs:
- Reduction of joint space , reflecting cartilage loss
- Osteophytes : bony growths visible on the edges of joints
- Subchondral sclerosis : densification of the underlying bone
- Geodes : small cavities filled with liquid
- Joint deformities : subluxations, misalignment of the fingers
X-rays also allow us to differentiate between the following shapes:
- Nodules clearly visible in nodular osteoarthritis
- Sharp, central erosions in erosive osteoarthritis
- Subluxation of the 1st metacarpal in CMC osteoarthritis of the thumb
MRI and ultrasound: targeted complementary tools
Magnetic resonance imaging (MRI) is not routine, but it can be useful in certain cases:
- Suspicion of associated ligament or tendon injury
- Unexplained pain with normal x-ray
- Preoperative assessment
It allows for detailed visualization of the cartilage, ligaments, synovial membrane and any associated lesions.
Joint ultrasound can also be used to:
- Detect effusion , synovitis or local inflammation
- Guide an infiltration (under ultrasound control)
- Assess vascularization in Doppler mode in erosive forms
These tools are particularly useful in differential diagnoses with inflammatory pathology or isolated tendon damage.
Biological analyses: eliminate inflammatory causes
Osteoarthritis is a non-systemic condition : in principle, blood tests are normal .
But in doubtful cases, particularly if the pain is nocturnal, very inflammatory, or asymmetrical, an assessment may be prescribed to exclude an inflammatory or autoimmune disease:
- VS, CRP : to detect active inflammation
- Rheumatoid factor, anti-CCP : in case of suspected rheumatoid arthritis
- Uricemia : in case of doubt with a gout attack
These tests make it possible to avoid missing a major differential diagnosis .
Arthroscopy: an exceptional tool
Rarely used for hand osteoarthritis, arthroscopy can , in certain complex or surgical cases, allow a direct assessment of the joint . It is also used to perform certain surgical procedures (debridement, joint cleaning).
Characteristic radiographic signs of hand osteoarthritis
Radiographic examination is one of the most widely used tools to confirm the diagnosis of osteoarthritis. It allows us to visualize structural changes in the joints, often well before symptoms become disabling. In the specific case of hand osteoarthritis, standard radiography remains the first-line examination : quick, inexpensive, available everywhere, and very revealing of the different phases of the disease.
But correctly interpreting the images requires a detailed understanding of the characteristic signs of this pathology. Because each visible abnormality tells a story of stress, repair, and remodeling—in short, the body’s attempt to adapt to wear and tear.
Joint space reduction: the fundamental marker
The most constant and earliest sign is the narrowing of the joint space . This reflects the progressive degeneration of cartilage , the tissue that normally covers bone surfaces, allowing them to slide without friction.
In hand osteoarthritis, this loss of cartilage can be:
- Focal (localized to one part of the joint)
- Global (affecting the entire articular surface)
The reduction in joint space is particularly clearly visible on frontal and oblique views, particularly at the level of:
- Distal interphalangeal (DI) joints
- Proximal interphalangeal (PI) joints
- From the carpo-metacarpal (CMC) of the thumb
This narrowing is often accompanied by a flattening or widening of the joint space , in an attempt to compensate.
Osteophytes: marginal bone growths
Osteophytes , also called “parrot beaks,” are bony growths that form on the edges of affected joints. They are the body’s adaptive response to joint instability: the bone attempts to “ strengthen” areas under abnormal stress.
In finger osteoarthritis, osteophytes are often clearly visible:
- At the ID level (Heberden)
- At the IP level (Bouchard)
- At the base of the thumb (CMC)
They sometimes give the joint an enlarged or deformed shape , visible even to the naked eye, and contribute to stiffness and functional limitation. Their size is not always proportional to the pain felt: some patients with large osteophytes have few symptoms, while others suffer with few visible signs.
Subchondral sclerosis: bone that becomes denser
In response to cartilage loss, the bone just below the joint (the subchondral bone ) may become denser and thicker. This phenomenon, called subchondral sclerosis , appears on X-rays as an increase in bone density in the immediate vicinity of the joint space.
It’s an adaptation mechanism: the bone attempts to withstand unusual mechanical stresses by strengthening itself. But this densification can make the bone more rigid, less able to absorb shocks, which aggravates mechanical pain.
Geodes (or subchondral cysts)
Another characteristic sign: the formation of geodes , small fluid-filled cavities located in the bone, just under the cartilage. They appear as radiolucent (blacker) areas on X-rays.
Geodes are the result of microfissures in the bone or excessive pressure that causes synovial fluid to penetrate the bone. They can be isolated or multiple, and are more common in advanced forms of osteoarthritis.
They are not always symptomatic, but their presence indicates an advanced stage of degeneration .
Joint deformation: the final impression
As the disease progresses, joint structures lose their natural alignment. Changes in joint shape and axis are observed :
- Lateral or angular deviations of the fingers
- Subluxations (partial displacement) of the bone heads
- Erasing the natural symmetry of line spacing
In erosive osteoarthritis or CMC involvement of the thumb, these deformations can be spectacular: widening of the base of the thumb , joint collapse , and a bad Z position . These alterations, once established, are irreversible and can seriously compromise function.
Radiological specificities according to clinical forms
| Form of osteoarthritis | Dominant radiographic signs |
|---|---|
| Nodular osteoarthritis | Osteophytes, progressive shrinkage, visible nodules |
| Erosive osteoarthritis | Central erosions, bone destruction, rapid deformation |
| CMC osteoarthritis of the thumb | Subluxation, osteophytes, joint collapse, saddle deformity |

Conventional medical treatments for hand osteoarthritis: what does conventional medicine offer?
Conventional medicine does not offer a curative treatment for hand osteoarthritis, but rather a therapeutic arsenal focused on reducing symptoms , improving function and preserving quality of life. The goal is to slow the progression of the disease , relieve pain and maintain joint mobility , while avoiding complications and loss of autonomy.
The choice of treatment depends on the stage of the disease , the clinical form (nodular, erosive, CMC of the thumb), the intensity of the symptoms , and the patient’s expectations . It is often based on a graded approach , ranging from conservative measures to more targeted interventions, or even surgery in severe forms.
Analgesic and anti-inflammatory treatments
Paracetamol
Paracetamol (acetaminophen) is often recommended as a first-line treatment for mild to moderate pain. It is well tolerated and can be used occasionally or regularly, but its effectiveness remains limited in advanced forms. It is mainly useful for relieving mechanical pain during use , without having a direct effect on inflammation.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs ( ibuprofen , naproxen, diclofenac, etc.) are indicated in cases of more intense pain or inflammatory flare-ups , particularly in erosive osteoarthritis. They can be prescribed orally , but also for local application (gels, creams), which reduces systemic adverse effects (digestive, renal or cardiovascular).
In elderly or polymedicated people, the topical route should be preferred to limit the risks.
Intra-articular infiltrations
In forms resistant to oral or local treatments, particularly for CMC osteoarthritis of the thumb, corticosteroid injections can provide temporary, sometimes dramatic, relief. They consist of injecting a powerful anti-inflammatory directly into the joint , under palpation or ultrasound control.
They are particularly useful in cases of:
- Acute disabling pain
- Major inflammation
- Contraindication to oral NSAIDs
However, their effect is often transient (a few weeks to a few months), and their repetition must be limited (2 to 3 per year), due to the risk of cartilage damage or infection.
Recent research is also exploring the use of hyaluronic acid injections (viscosupplementation), but the results in the small joints of the hand remain unconvincing.
Resting orthoses and splints
Functional or resting orthoses , prescribed by a doctor or made by an occupational therapist, are particularly recommended for thumb osteoarthritis (CMC) or during painful flare-ups. They have several objectives:
- Stabilize the painful joint
- Limit traumatic movements
- Reduce inflammation
- Preserve joint range of motion
They can be worn:
- At night , to limit nocturnal microtraumas
- During the day, during specific activities
Thermoformed splints offer superior comfort and can be adjusted as symptoms change. Patient compliance with regular use of the brace is a key factor in their effectiveness.
Physiotherapy and occupational therapy
Functional rehabilitation plays a major role in maintaining joint mobility , preserving muscle strength , and preventing deformities . The physiotherapist or occupational therapist guides the patient through:
- Gentle active exercises to maintain flexibility
- Targeted muscle strengthening
- Relaxing massages
- Painless passive mobilizations
In occupational therapy, the emphasis is on:
- Adapting daily gestures
- The use of technical aids (jar openers, ergonomic pens)
- Learning protective postures
The alliance between these two disciplines makes it possible to limit the development of stiffness, ankylosis or excessive compensation.
Surgical treatments (as a last resort)
Surgery is only considered in severe and very disabling forms , after failure of conservative treatments. It is most often proposed for CMC osteoarthritis of the thumb, when there is marked deformity , chronic pain , and major loss of function .
Techniques include:
- Trapeziectomy (removal of the trapezius)
- Arthroplasty (installation of a prosthesis)
- Arthrodesis (joint fusion)
These interventions can restore some function, but they involve a long rehabilitation period and variable results depending on the initial joint condition.
The osteopathic approach in the management of hand osteoarthritis
Hand osteoarthritis, although part of a logic of progressive joint degeneration, is not reduced to mechanical wear. It is the expression of a local and global imbalance, in a body that compensates, adapts, then exhausts itself. In this context, osteopathy offers a profoundly complementary approach , centered on the quality of movement , tissue harmony , and listening to the person as a whole .
Far from claiming to “repair” damaged cartilage, the osteopath seeks to make the joint environment more fluid , to reduce mechanical constraints , and to stimulate self-regulation mechanisms to slow down the progression and improve functional comfort.
Restore local joint mobility
In osteoarthritis, one of the key objectives is to preserve, or even restore, joint mobility . As stiffness sets in, the osteopath mobilizes the surrounding structures in a gentle and respectful manner, without forcing the already altered joints.
The techniques used are generally:
- Gentle joints (rhythmic mobilizations, oscillations)
- Indirect , by working the periarticular soft tissues
- Myotensives , to release muscle tension around the fingers
- Decoaptation , when the joint is compressed or loses elasticity
The challenge is to reduce adhesions , promote pain-free range of motion , and maintain the fundamental micro-movements that allow natural lubrication of the joint.
Release tissue constraints remotely
Osteopathy considers the hand as an extension of a larger functional chain . Stress on the shoulder, loss of mobility at the elbow or an overall postural imbalance can increase tension on the hand , and thus aggravate osteoarthritic symptoms.
The osteopath therefore examines:
- The upper limb as a whole (shoulder, arm, elbow, wrist)
- The shoulder and cervical girdle , often linked to postural compensations
- The descending myofascial chain (linked to spinal tension or support)
By working on these areas remotely, it becomes possible to reduce the functional load carried by the joints of the hand, and to rebalance everyday movements .
Improve local circulation and drainage
Osteoarthritis is often accompanied by a slowdown in metabolic exchanges in joint tissues. Decreased oxygenation, venous or lymphatic stagnation, or the accumulation of pro-inflammatory mediators maintain pain and stiffness.
The osteopath then acts on:
- The local vascular system (pumping techniques, gentle drainage)
- The lymphatic system , particularly in the axilla and thorax
- Thoracic breathing , the natural engine of circulation
This gentle stimulation promotes better nutrition of the residual cartilage , evacuation of metabolic waste , and relief of congested areas .
Supporting psycho-corporal adaptation
Osteopathy, in its holistic dimension, considers that the bodily experience of a joint pathology influences the patient’s feelings, posture, and coping skills. Osteoarthritis of the hand, because it limits meaningful gestures (touching, holding, creating, giving), can resonate with deeper tensions—affective, identity-related, or emotional.
In this context, the osteopath can:
- Welcoming the emotional feelings associated with loss of function
- Offer a safe space for body listening
- Work on somato-emotional compensation areas (diaphragm, occiput, thorax)
This sensitive approach helps to reintegrate the hand into the body schema and to restore a form of confidence in the gesture.
Practical advice and preventive measures
Osteopathy doesn’t stop at the treatment table. It is accompanied by personalized recommendations :
- Gentle self-mobilization exercises for the fingers and wrist
- Local hydrotherapy (hot/cold alternation, paraffin baths)
- Adaptation of the workstation or repetitive movements
- Tips on everyday ergonomics : handles, utensils, tools
The osteopath plays the role of an educator of gesture , helping the patient to preserve their function in a dynamic of active prevention.
Exercises and self-management tips to maintain hand mobility
Hand osteoarthritis can feel like the body is closing in on itself, like a joint that stiffens, contracts, and gives way. However, even if the wear and tear on the cartilage is irreversible, movement remains an essential key to maintaining flexibility, limiting pain, and regaining a form of functional freedom. Far from intense exertion, it is often simple, regular movements that respect the body’s rhythm that produce the most lasting effects.
In this section, we offer gentle exercises and practical advice to maintain mobility, strengthen muscles, improve local circulation and promote a more peaceful relationship with your hands on a daily basis.
Basic rule: listen to the hand, never force
First and foremost, every exercise should be performed pain-free . A slight tension or moderate stretch is acceptable, but if a joint becomes red, swollen, or painful after the exercise, it is either too intense or not appropriate.Ideal frequency: 1 to 2 times a day , 5 to 10 minutes is enoughOptimal conditions: warm hand (warm bath, gentle friction), calm environment, relaxed breathing
Overall joint warm-upWrist rolls
- Join hands as if in prayer
- Make small circles in one direction, then the other.
- Duration: 30 seconds on each side
→ Goal : stimulate the synovium, improve joint lubrication - Gentle friction
- Massage the fingers, one by one, from the base to the tip
- Gently press on painful areas
- Use a vegetable oil if necessary (arnica, calendula)
→ Purpose : relax soft tissues, activate local circulation
Mobility and flexibility exercisesProgressive opening/closing
- Open your hand slowly, spreading your fingers wide apart
- Close your hand gently, trying to touch the palm with each finger.
- Repeat 10 times
→ Goal : maintain joint range of motion and avoid tendon retraction - Finger fanning
- Place your hand flat on a table
- Spread your fingers as far apart as possible, then gently bring them together
- Repeat 10 times
→ Goal : to promote digital independence and fine coordination - Thumb mobilization
Gentle strengthening and proprioception
Light pressure in a soft ball
- Use a foam ball or sponge
- Press slowly, hold for 3 seconds, release
- Repeat 8 to 10 times
→ Goal : maintain strength without stressing the joints
Thumb-index clip
- Press a small, soft object (cotton ball, rolled up cloth) between your thumb and another finger
- Alternate fingers, hold for a few seconds
→ Goal : strengthen fine grip
Stretching and releasingDorsal finger stretch
- Hand outstretched palm up
- With the other hand, gently pull the fingers towards the floor
- Hold for 20 seconds, release
→ Goal : Relieve flexor tension and open joints
Paraffin bath or hot compresses
- Soak hands in a warm bath (35–38°C) for 10 minutes
- Dry gently, then perform the exercises
→ Goal : to soften the tissues before mobilization
Practical self-management tips
Adapt daily gestures
- Favor straight line movements , avoid sudden twists
- Use both hands to carry or lift objects
- Alternate tasks to avoid repetition
Home ergonomics
- Use utensils with thick handles
- Install an automatic jar opener
- Prefer wide pens and suitable (ergonomic) cutleryAvoid periods of prolonged immobility
- Move your fingers every 30–60 minutes, even while sitting
- Incorporate mini-gestures into the routine: folding/unfolding in front of the television, in transport, etc.
Natural complementary tips
- Massage with essential oils : wintergreen, lemon eucalyptus or true lavender diluted in a vegetable oil
- Anti-inflammatory infusions : turmeric, ginger, nettle
- Diet rich in omega-3 , antioxidants, natural collagen
Food and nutritional support
Diet plays an often underestimated role in the management of hand osteoarthritis. While it cannot regenerate already damaged cartilage, it is an important lever for modulating inflammation, nourishing joint tissues, and supporting tissue repair processes. A targeted diet can help reduce pain, slow lesion progression, and promote a more favorable biological environment for joint mobility.
Some pro-inflammatory substances, such as cytokines or prostaglandins, are directly influenced by dietary intake. Conversely, several nutrients have anti-inflammatory, antioxidant, or chondroprotective properties, which can alleviate osteoarthritis symptoms. The goal is not to “cure through diet,” but to provide the body with a biochemical environment that limits the worsening of the disease.
Omega-3s are the undisputed stars of the anti-inflammatory diet. These polyunsaturated fatty acids, found particularly in oily fish (sardines, mackerel, wild salmon), flaxseeds, walnuts, and rapeseed oil, have been shown to inhibit inflammatory mediators. Several studies suggest that their regular consumption can reduce pain and morning stiffness in people with osteoarthritis. Fish oil supplements can also be considered, under medical supervision, especially in cases of proven deficiency.
Antioxidants play another central role. By neutralizing free radicals produced during oxidative stress (a common phenomenon in osteoarthritis), they help limit cellular damage. Vitamins C and E, zinc, selenium, and polyphenols (found in red fruits, green tea, turmeric, and raw cocoa) are valuable allies. They are found in berries, citrus fruits, spinach, artichokes, broccoli, and spices like ginger and turmeric, which combine antioxidant and natural anti-inflammatory properties.
Turmeric, in particular, is being studied for its main active ingredient, curcumin, which is known for its anti-inflammatory properties. To optimize its absorption, it is recommended to combine it with a fatty substance (olive or coconut oil) and piperine (a component of black pepper). Standardized curcumin extracts as a dietary supplement may also be recommended for more advanced cases.
Collagen, the main component of cartilage and connective tissue, deserves special attention. With age, endogenous collagen synthesis declines, weakening joint structures. A diet containing bone broth, whole fish (with skin and bones), or hydrolyzed collagen supplements can support connective tissue regeneration and improve the quality of residual cartilage. Some formulas enriched with hyaluronic acid or vitamin C (essential for collagen synthesis) are even more effective.
The overall diet should aim to reduce low-grade inflammation. This means limiting the consumption of processed foods rich in refined sugars, trans fatty acids, and additives, which promote the production of pro-inflammatory substances. Excessive consumption of red meat, processed meats, industrial dairy products, and alcohol should also be avoided as a joint support approach. Conversely, Mediterranean-style diets, rich in colorful vegetables, legumes, whole grains, fresh herbs, fish, and healthy fats, have been shown to be effective in preventing chronic inflammatory conditions, including osteoarthritis.
Hydration remains essential. Cartilage is an avascular tissue that depends on synovial fluid exchange for its metabolism. Proper hydration promotes joint lubrication and limits tissue dehydration. Drinking enough water, limiting sugary or stimulant drinks (coffee, sodas), and favoring anti-inflammatory herbal teas (nettle, meadowsweet, ash) are among the simple but powerful actions.
Some specific nutritional supplements may be offered depending on the patient’s profile: glucosamine, chondroitin, MSM (methylsulfonylmethane), organic silica, or amino acids such as glycine or proline. Their effectiveness varies from one individual to another, and they should never replace a healthy diet, but should be added to it in a targeted and temporary manner, within a supervised integrative approach.
Finally, it’s essential to remember that nutrition shouldn’t be a source of frustration or rigidity. It’s not about adopting a strict diet, but about gradually evolving your habits toward a nourishing, anti-inflammatory, vibrant, and sustainable model. Regularity and consistency are more important than perfection.
Preventing Finger Osteoarthritis: Simple Actions and Protective Habits
Hand osteoarthritis is not an inevitable age-related condition. While genetic or hormonal factors can promote its onset, many lifestyle factors influence its progression, or even its prevention. Preventing osteoarthritis means protecting your joint health as soon as possible by adopting habits that respect your body, particularly your hands, which are often overused, neglected, or used inappropriately.
Our fingers, wrists, and thumbs are used daily in often repetitive, sometimes unconscious, tasks: typing on a keyboard, tightening objects, cooking, DIY, lifting, and massaging. This repetition of movements, when not balanced or compensated, can lead to micro-lesions, chronic stress, and muscle imbalances that, in the long term, weaken joint structures. This is why gesture education, postural prevention, and effort modulation are essential pillars for preserving hand joint health.
One of the simplest preventative measures is varying postures and grips. When performing prolonged manual tasks (sewing, gardening, computer work, driving), it’s beneficial to change positions regularly, alternate hands if possible, or take micro-breaks every 20 to 30 minutes to move your fingers in all directions. These active breaks rehydrate cartilage, lubricate joints, and prevent numbness that indicates vascular or nerve compression.
Ergonomics also plays a crucial role. Much pain associated with hand overuse could be avoided by adapting tools to the capabilities of the fingers. This includes wide, flexible pens, non-slip handles, assisted jar openers, ergonomic scissors, or height-adjustable keyboards. Small hardware changes can significantly reduce repetitive joint stress.
Particular attention should be paid to the thumb, which is particularly exposed in forms of CMC osteoarthritis. Avoiding holding the hand in a tight pinch for long periods, distributing the force across the entire palm and involving all the fingers in the effort helps to better balance the pressure. In high-risk professional activities (hairdressing, crafts, musicians, manual workers), specific preventative work with a therapist can be valuable in correcting harmful automatic gestures.
Gentle muscle strengthening is another important area of prevention. Maintaining the tone of the forearm, interosseous, and lumbrical muscles (intrinsic muscles of the hand) stabilizes joints, limits hyperlaxity, and cushions mechanical stress. Simple exercises, performed regularly (pressure on a soft ball, thumb-index pinch, finger spreaders) help create a more stable and better oxygenated joint environment.
Stress management is often overlooked in joint prevention. Yet, emotional tension frequently manifests as involuntary clenching, clenched fists, or rigid hand positions. These chronic micro-contractures, when left unexpressed, can fuel a silent inflammation. Practices such as yoga, mindfulness meditation, Qigong, or self-massage can help relax these reflexive tensions and restore a gentler, more conscious relationship with the hands.
Exposure to cold is also an aggravating factor to consider. Hands frequently exposed to the cold without protection can cause their microcirculation to contract, which slows tissue nutrition and promotes stiffness. It is advisable to wear gloves outdoors in cold weather, or to use warm compresses at the end of the day if fingers are sensitive or painful.
Finally, prevention involves physical education from childhood. Encouraging children to engage in a variety of manual activities, balancing screen time with skill-based games, and avoiding overuse of a single finger (such as the thumb on a cell phone) are all useful reflexes for preserving future joint health. Because prevention isn’t limited to the elderly: it’s a lifelong movement hygiene.
Preventing finger osteoarthritis: simple actions and protective habits
Hand osteoarthritis is not an inevitable, age-related inevitability. While genetic or hormonal factors can contribute to its onset, many lifestyle factors influence its progression and even its prevention. Preventing osteoarthritis means protecting your joint health as early as possible by adopting habits that respect your body, particularly your hands, which are often overused, neglected, or misused.
Our fingers, wrists, and thumbs are used daily in often repetitive, sometimes unconscious, tasks: typing on a keyboard, tightening objects, cooking, DIY, lifting, and massaging. This repetition of movements, when not balanced or compensated, can lead to micro-lesions, chronic stress, and muscle imbalances that, in the long term, weaken joint structures. This is why gesture education, postural prevention, and effort modulation are essential pillars for preserving hand joint health.
One of the simplest preventative measures is varying postures and grips . When performing prolonged manual tasks (sewing, gardening, computer work, driving), it is beneficial to regularly change positions, alternate hands if possible, or take micro-breaks every 20 to 30 minutes to move your fingers in all directions. These active breaks rehydrate the cartilage, lubricate the joints, and prevent numbness that indicates vascular or nerve compression.
Ergonomics also plays a crucial role. Much pain associated with hand overuse could be avoided by adapting tools to the capabilities of the fingers. This includes wide, flexible pens, non-slip handles, assisted jar openers, ergonomic scissors, or height-adjustable keyboards. Small hardware changes can significantly reduce repetitive joint stress.
Particular attention should be paid to the thumb , which is particularly exposed in forms of CMC osteoarthritis. Avoiding holding the hand in a tight pinch for long periods, distributing the force over the entire palm and involving all the fingers in the efforts helps to better balance the pressure. In high-risk professional activities (hairdressing, crafts, musicians, manual workers), specific preventive work with a therapist can be valuable in correcting harmful automatic gestures.
Gentle muscle strengthening is another important area of prevention. Maintaining the tone of the forearm, interosseous, and lumbrical muscles (intrinsic muscles of the hand) stabilizes joints, limits hyperlaxity, and cushions mechanical stress. Simple exercises, performed regularly (pressure on a soft ball, thumb-index pinch, finger spreaders) help create a more stable and better oxygenated joint environment.
Stress management is often overlooked in joint prevention. Yet, emotional tension frequently manifests as involuntary clenching, clenched fists, or rigid hand positions. These chronic micro-contractures, when left unexpressed, can fuel a silent inflammation. Practices such as yoga, mindfulness meditation, Qigong, or self-massage can help relax these reflexive tensions and restore a gentler, more conscious relationship with the hands.
Exposure to cold is also an aggravating factor to consider. Hands frequently exposed to the cold without protection can cause their microcirculation to contract, which slows tissue nutrition and promotes stiffness. It is advisable to wear gloves outdoors in cold weather, or to use warm compresses at the end of the day if fingers are sensitive or painful.
Finally, prevention involves physical education from childhood. Encouraging children to engage in a variety of manual activities, balancing screen time with skill-based games, and avoiding overuse of a single finger (such as the thumb on a cell phone) are all useful reflexes for preserving future joint health. Because prevention isn’t limited to the elderly: it’s a lifelong movement hygiene.
What current research tells us
Over the past two decades, our understanding of osteoarthritis has evolved profoundly. Far from being perceived as a simple consequence of aging or mechanical wear of the joints, hand osteoarthritis is now considered a complex, multifactorial, and dynamic pathology , combining low-grade inflammation, tissue remodeling, metabolic imbalances, and genetic influences. Recent research has helped refine our view of the mechanisms at work, but also of promising therapeutic avenues, whether conventional or complementary.
One of the major breakthroughs brought about by research concerns the role of silent inflammation in the development and progression of osteoarthritis. Contrary to the long-held belief that this condition is purely degenerative, numerous studies have shown that subtle but chronic inflammatory processes are present from the early stages, particularly in the synovial membrane. This low-grade inflammation contributes to cartilage degradation, osteophyte proliferation, and pain. It paves the way for new anti-inflammatory approaches, not only medication-based but also nutritional or behavioral.
Furthermore, medical imaging research has transformed our ability to detect and characterize hand osteoarthritis. MRI and high-resolution ultrasound now make it possible to visualize cartilage lesions, bone remodeling, but also synovitis and early intra-articular effusions. These tools show that the intensity of symptoms is not always correlated with the extent of anatomical lesions visible on standard radiographs. This dissociation between structure and pain encourages care centered on the person and their experience , rather than solely on images.
Research has also highlighted the role of hormonal factors in hand osteoarthritis, particularly in women. After menopause, the drop in estrogen levels appears to promote the appearance of Heberden and Bouchard nodules, as well as a more rapid progression of joint degeneration. This observation has led to exploration of the effect of hormone replacement therapy on preventing or stabilizing digital osteoarthritis, with results that are still debated but promising.
On the therapeutic front, targeted biotherapies are the subject of active research. Certain monoclonal antibodies targeting interleukins (such as IL-1 or IL-6), as well as metalloprotease inhibitors or modulators of chondrocyte activity, are currently being evaluated. Although these treatments are still far from common use for hand osteoarthritis, they reflect a paradigm shift: treating not only the symptoms, but the underlying biological mechanisms.
At the same time, research is increasingly exploring integrative approaches . Several studies have evaluated the effects of yoga, acupuncture, mindfulness meditation, or gentle physiotherapy in reducing pain and improving manual function. Osteopathy, although less studied specifically for arthritic hands, benefits from work showing the positive impact of manual techniques on pain, mobility, and quality of life in chronic musculoskeletal disorders. These non-drug approaches are all the more interesting because they are minimally invasive, respectful of the patient’s rhythm , and can be combined with other treatments.
The literature on nutrition applied to osteoarthritis has also grown. Several clinical trials have shown the benefits of omega-3, turmeric (curcumin), avocado/soy extracts (ASU), and glucosamine and chondroitin in reducing osteoarthritis pain, particularly in the hands. However, the effects are often moderate and vary between individuals, which underlines the importance of personalized support .
Finally, neuroscience research reminds us that osteoarthritis pain is not only peripheral . It also involves central sensitization: the brain can maintain the perception of pain even in the absence of proportional damage. This phenomenon explains why some patients retain intense pain despite little degradation of images, or conversely, remain minimally symptomatic despite advanced osteoarthritis. This reinforces the interest of holistic approaches integrating the emotional, perceptual and sensory dimensions of the painful experience.
Thus, current research, by combining the perspectives of biology, clinical practice, technology and human sciences, enriches our understanding of hand osteoarthritis. It confirms that the best strategy remains multidisciplinary, progressive, and centered on the person as a whole .
References
- Fife R S. Osteoarthritis ‐ epidemiology, pathology, and pathogenesis. Primer on the Rheumatic Diseases, 11th ed. Atlanta, Georgia: Arthritis Foundation, 1997216–217.
- Hochberg M C. Osteoarthritis ‐ clinical features and treatment. Primer on the Rheumatic Diseases, 11th edn. Atlanta, Georgia: Arthritis Foundation, 1997218–221.
- Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K.et al The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand. Arthritis Rheum 1990331601–1610. [PubMed] [Google Scholar]
- Bijkerk C. Assessment of radiological osteoarthritis in peripheral joints and of disk degeneration of the spine. Thesis 199917–32.
- Cushnagan J, Dieppe P. Study of 500 patients with limb joint osteoarthritis. I. Analysis by age, sex, and distribution of symptomatic joint sites. Ann Rheum Dis 1991508–13. [PMC free article] [PubMed] [Google Scholar]
- Egger P, Cooper C, Hart D J, Doyle D V, Coggon D, Spector T D. Patterns of joint involvement in osteoarthritis of the hands: the Chingford study. J Rheumatol 1995221509–1513. [PubMed] [Google Scholar]
- Niu J, Zhang Y, LaValley M, Chaisson C E, Aliabadi P, Felson D T. Symmetry and clustering of symptomatic hand osteoarthritis in elderly men and women: the Framingham Study. Rheumatology 200342343–348. [PubMed] [Google Scholar]
- Poole J, Sayer A A, Hardy R, Wadsdorth M, Kuh D, Cooper C. Patterns of interphalangeal hand joint involvement of osteoarthritis among men and women. A British cohort study. Arthritis Rheum 2003483371–3376. [PubMed] [Google Scholar]
- Cooper C, Egger P, Coggon D, Hart D J, Masud T, Cicuttini F.et al Generalized osteoarthritis in women: pattern of joint involvement and approaches to definition for epidemiological studies. J Rheumatol 1996231938–1942. [PubMed] [Google Scholar]
- Hunter D J, Demissie S, Cupples L A, Aliabadi P, Felson D T. A genome scan for joint‐specific hand osteoarthritis susceptibility. The Framingham study. Arthritis Rheum 2004502489–2496. [PubMed] [Google Scholar]
- Dougados M, Nakache JP, Gueguen A. Criteria for generalized and focal osteoarthritis. Rev Rhum 199663569–575. [ PubMed ] [ Google Scholar
- Kellgren J H, Moore R. Generalized osteoarthritis and Heberden’s nodes. BMJ 19521181–187. [PMC free article] [PubMed] [Google Scholar]
- Lawrence J S. Generalized osteoarthrosis in a population sample. Amer J Epid 196390381–389. [PubMed] [Google Scholar]
- Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K.et al Development of criteria for the classification and reporting of osteoarthritis of the knee. Arthritis Rheum 1986291039–1049. [PubMed] [Google Scholar]
- Slatkowsky‐Christensen B, Kvien T K, Bellamy N. Performance of the Norwegian version of AUSCAN – disease‐specific measure of hand osteoarthritis. Osteoarthritis Cartilage 200513561–567. [PubMed] [Google Scholar]
- Petersson I F, Jacobsson L T H. Osteoarthritis of the peripheral joints. Best Pract Res Clin Rheumatol 200216741–760. [PubMed] [Google Scholar]
- Bagge E, Bjelle A, Eden S, Svanborg A. A longitudinal study of the occurrence of joint complaints in elderly people. Age Ageing 199221160–167. [PubMed] [Google Scholar]
- Van Saase J L, van Romunde L K J, Cats A, Vandenbroucke J P, Valkenburg H A. Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann Rheum Dis 198948271–280. [PMC free article] [PubMed] [Google Scholar]
- Bagge E, Bjelle A, Svanborg A. Radiographic osteoarthritis in the elderly. A cohort comparison and a longitudinal study of the “70‐year old people in Goteborg”. Clin Rheumatol 199211486–491. [PubMed] [Google Scholar]
- Bagge E, Bjelle A, Eden S, Svanborg A. Factors associated with radiographic osteoarthritis: results from the population study 70‐year‐old people in Goteborg. J Rheumatol 1991181218–1222. [PubMed] [Google Scholar]
- Carman W J, Sowers M, Hawthorne V M, Weissfeld L A. Obesity as a risk factor for osteoarthritis of the hand and wrist: a prospective study. Am J Epidemiol 1994139119–129. [PubMed] [Google Scholar]
- Lawrence J S.Rheumatism in populations. London: Heineman, 1977
- Chaisson C E, Zhang Y, Sharma L, Kannel W, Felson D T. Grip strength and the risk of developing radiographic hand osteoarthritis: results from the Framingham Study. Arthritis Rheum 19994233–38. [PubMed] [Google Scholar]
- Stecher R M. Heberden’s nodes: heredity in hypertrophic arthritis of finger joints. Am J Med Sci 1941201801–809. [Google Scholar]
- Riyazi N, Meulenbelt I, Kroon H M, Ronday H K, le Graverand Hellio, Rosendaal F R.et al Evidence for familial aggregation of hand, hip, and spine but not knee osteoarthritis in siblings with multiple joint involvement: the GARP study. Ann Rheum Dis 200564438–443. [PMC free article] [PubMed] [Google Scholar]
- Knowlton R G, Katzenstein P L, Moskowitz R W, Weaver E J, Malemud C J, Pathria M N.et al Genetic linkage of a polymorphism in the type II procollagen gene (COL2A1) to primary osteoarthritis associated with mild chondrodysplasia. N Engl J Med 1990322526–530. [PubMed] [Google Scholar]
- Stefansson S E, Jonsson H, Ingvarsson T, Manolescu I, Jonsson H H, Olafsdottir G.et al Genomewide scan for hand osteoarthritis: a novel mutation in matrilin‐3. Am J Hum Genet 2003721448–1459. [PMC free article] [PubMed] [Google Scholar]