Introduction
Osteoporosis, often referred to as the silent epidemic, is a disease condition characterized by a decrease in bone mass per unit volume, resulting from the loss of bone proteins. This disorder is manifested by a disruption of the bone remodeling process, marked by an increase in bone resorption which does not correspond to a parallel increase in bone formation.
Known as the “silent thief,” osteoporosis operates insidiously, often without obvious symptoms. This insidious disease can progress silently over several years, eroding bone density and increasing the risk of fractures. Unfortunately, the silent nature of osteoporosis makes it difficult to detect, and it often goes unrecognized until a fracture occurs, usually in the hip, ribs, or spine.
Bone fragility resulting from osteoporosis is of particular concern due to its serious health consequences. Hip fractures, for example, are associated with significant morbidity and mortality, particularly among older adults. These fractures can lead to loss of independence, medical complications, and reduced quality of life.
Osteoporosis primarily affects postmenopausal women due to the hormonal changes associated with this time of life. However, it can also affect men and other population groups, particularly those with risk factors such as calcium deficiency, vitamin D deficiency, smoking, physical inactivity, and prolonged use of certain drugs.
Diagnosis of osteoporosis is often based on bone density tests, which can assess bone mineral density and identify people at increased risk of fractures. However, it is crucial to raise awareness about the prevention and management of this disease well before it progresses to an advanced stage. Preventative measures include eating a diet rich in calcium and vitamin D, exercising regularly to strengthen bones and improve balance, and avoiding harmful behaviors such as smoking and excessive consumption of drugs. ‘alcohol.
Treatment of osteoporosis often aims to slow bone loss, strengthen existing bone mass, and reduce the risk of fractures. It may involve the use of specific medications, nutritional supplements, and regular medical monitoring.
Thus, osteoporosis represents a major public health challenge, affecting the quality of life of individuals and leading to serious complications. As a “silent thief,” she reiterates the importance of prevention and awareness to identify and treat this disease before it causes irreversible damage. Continued research in the field of bone health is crucial to developing more effective approaches to the prevention and treatment of osteoporosis, in order to improve the bone health of the global population.
The shrinkage of bone cells (osteoclasts) is greater than the activity of the cells that form bone (osteoblasts)
The stiffness of a bone is directly proportional to its calcium concentration. Osteoblasts are the cells responsible for the formation of osteons, thus constituting bone tissue, while osteoclasts are responsible for its resorption. In children, frequent remodeling of bone structure is essential to promote growth. Bone is a dynamic tissue, undergoing a constant process of bone remodeling that involves both bone resorption and bone production throughout life.
On the other hand, in adults, it may happen that the activity of osteoclasts predominates over that of osteoblasts. In these cases, the bone mass loses its strength, thus becoming prone to fractures.
Osteoclasts are responsible for bone resorption, involving the breakdown and removal of bone tissue, while osteoblasts are responsible for the formation of new bone. In the context of osteoporosis, an imbalance between these two processes typically manifests as increased osteoclast activity, leading to a net loss of bone tissue over time. This imbalance can result from various factors such as aging, hormonal changes (including decreases in sex hormones like estrogen in postmenopausal women), calcium or vitamin D deficiency, and other genetic or environmental factors. .
Treatment of osteoporosis often aims to restore the balance between bone formation and resorption. This may involve lifestyle adjustments, such as eating a diet rich in calcium and vitamin D, doing muscle-strengthening exercises regularly, and managing risk factors. In some cases, medications may be prescribed to stimulate bone formation or inhibit bone resorption. It is crucial to consult a healthcare professional to obtain an accurate diagnosis and develop a suitable treatment plan for osteoporosis.
Osteoclast
Bone cells responsible for the resorption of bone tissue and therefore participating in its continuous renewal.

Osteoblast
Bone cells responsible for the deposition of bone tissue

Characteristics of Osteoporosis
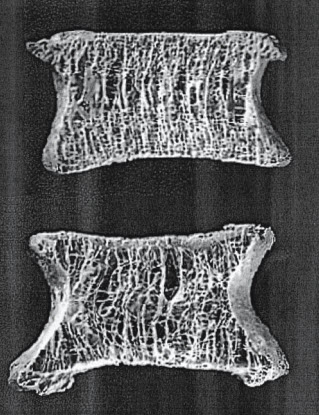
Osteoporosis is a progressive bone disease characterized by a reduction in bone mass and deterioration of bone tissue, leading to increased fragility and a higher risk of fractures. Although it is often considered a “silent” disease because bone loss occurs without symptoms, its impact becomes significant when a fracture occurs. The structural integrity of bones is compromised in various ways due to osteoporosis. Below are some of the key characteristics of osteoporosis, focusing on changes in bone microarchitecture, particularly in the trabecular bone.
List of Characteristics
1. Reduction in the Number of Trabeculae
One of the most important structural changes in osteoporosis is the reduction in the number of trabeculae. Trabeculae are the fine, lattice-like structures found inside bones, especially in areas rich in trabecular bone, like the spine, hips, and wrists. These small, interconnected rods and plates help bones absorb and distribute the stresses placed on them. However, in osteoporosis, the number of trabeculae begins to decrease, which compromises the bone’s internal support framework.
- Impact: Fewer trabeculae mean that the bone’s ability to handle everyday loads, such as walking, standing, or even minor impacts, is diminished. This reduction weakens the bone, making it more susceptible to fractures, particularly in load-bearing bones like the spine and hips.
- Outcome: As the number of trabeculae decreases, the remaining structure struggles to distribute weight and impact effectively, leading to fractures that might occur with minimal trauma.
2. Reduced Trabecular Thickness
In addition to the decrease in the number of trabeculae, there is also a reduction in trabecular thickness. Healthy trabeculae are thick enough to support the stresses that bones endure daily. However, with osteoporosis, the trabeculae become thinner and more fragile, reducing the bone’s overall ability to withstand loads.
- Impact: Thinner trabeculae lose their ability to support the loads that bones typically bear. With reduced thickness, the remaining trabecular network becomes too fragile to effectively perform its function, increasing the risk of fractures. For instance, even activities like bending over or lifting a light object can lead to fractures in people with osteoporosis.
- Outcome: The weakening of trabeculae leaves the bone structurally unsound, causing it to become prone to collapsing under normal stresses. This can lead to compression fractures in the spine, hip fractures, or wrist fractures.
3. Reduced Trabecular Connectivity
Another hallmark characteristic of osteoporosis is the reduction in trabecular connectivity. In healthy bone, trabeculae are interconnected, forming a network that helps distribute forces evenly across the bone. In osteoporosis, however, this connectivity is disrupted, further reducing the bone’s strength and integrity.
- Impact: Loss of trabecular connectivity means that the remaining trabeculae are not able to support each other as effectively, which compromises the bone’s ability to maintain its shape and strength. This lack of cohesion leads to a situation where the bone’s structural integrity is compromised, increasing the likelihood of fractures.
- Outcome: With the loss of trabecular connections, the bone becomes more prone to fractures. Each fracture weakens the overall structure, leading to a vicious cycle where one fracture makes further fractures more likely. This is particularly evident in spinal compression fractures, where multiple fractures lead to spinal deformities like kyphosis (a hunched back).
4. Cortical Bone Changes
While trabecular bone is most affected by osteoporosis, cortical bone (the dense outer layer of bone) also undergoes significant changes. The thinning of cortical bone contributes to the overall weakening of the skeleton. Although cortical bone is not as metabolically active as trabecular bone, the reduction in thickness can still have serious consequences for bone strength and fracture risk.
- Impact: Thinning of the cortical bone means that bones are less capable of resisting fractures from external forces. This is particularly problematic in areas like the femur (thigh bone), where fractures can lead to long-term disability or even death in elderly patients.
- Outcome: A decrease in cortical bone density and thickness makes bones more fragile, particularly in the hips and wrists, which are common sites for fractures in osteoporotic patients.
5. Increased Porosity of Bone
Osteoporosis also leads to an increase in bone porosity, meaning that the bones have larger and more numerous holes or spaces. This change is primarily a result of the loss of trabeculae and thinning of cortical bone.
- Impact: The increased porosity of bones further weakens their structure. Porous bones are less able to support weight and are more prone to fractures, even from low-impact activities such as walking or minor falls.
- Outcome: Increased bone porosity, combined with reduced trabecular thickness and connectivity, leaves bones highly vulnerable to fractures. Patients with osteoporosis are at an elevated risk of fragility fractures, which occur with minimal or no trauma.
6. Loss of Bone Mass
Osteoporosis is fundamentally characterized by a loss of bone mass. This reduction in mass occurs because the balance between bone resorption (the process of breaking down bone) and bone formation is disrupted. Normally, bone is constantly being remodeled, with old bone being removed and replaced with new bone. In osteoporosis, the rate of bone resorption exceeds the rate of bone formation, leading to a net loss of bone mass.
- Impact: This overall reduction in bone mass weakens the skeleton, making it more prone to fractures, particularly in bones that carry a significant load, such as the spine, hips, and wrists.
- Outcome: As bone mass decreases, fractures occur more easily, even from minor falls or simple movements. The loss of bone mass is often detected using a bone mineral density (BMD) test, such as a DEXA scan, which is a diagnostic tool for osteoporosis.
7. Microarchitectural Deterioration
One of the more subtle but critical features of osteoporosis is the deterioration of the bone’s microarchitecture. This means that the internal structure of the bone, including the trabeculae, is compromised, making it less able to withstand mechanical loads and impacts.
- Impact: Even if bone mass is only moderately reduced, the loss of microarchitectural integrity significantly increases fracture risk. Bones that have lost their intricate, lattice-like structure are much weaker, even if they still retain a significant amount of bone mass.
- Outcome: This microarchitectural deterioration is particularly dangerous because it’s not always detectable through standard bone density measurements. Patients with moderate bone density loss but severe microarchitectural deterioration may still be at high risk of fractures.
8. Cortical Porosity
While osteoporosis is often thought of as primarily affecting trabecular bone (the spongy bone inside the vertebrae and ends of long bones), cortical bone (the dense outer layer) also becomes porous with age and bone loss. This cortical porosity contributes to the overall weakening of the bone.
- Impact: The increased porosity of cortical bone weakens its ability to provide structural support. Cortical bone becomes more fragile as it becomes thinner and filled with small holes or cavities, which compromise its mechanical properties.
- Outcome: Cortical porosity leads to fractures in long bones like the femur (thigh bone), especially in older adults. These fractures, such as hip fractures, are particularly dangerous because they often lead to long-term disability or even death in elderly patients.
9. Impaired Bone Remodeling
In osteoporosis, the balance between osteoclasts (cells that break down bone) and osteoblasts (cells that form new bone) is disrupted, leading to impaired bone remodeling. Normally, bone is a dynamic tissue that is constantly being broken down and rebuilt in response to stress and other factors.
- Impact: In osteoporosis, bone resorption by osteoclasts is increased, while bone formation by osteoblasts is reduced or inefficient. This imbalance leads to a net loss of bone over time.
- Outcome: Impaired bone remodeling is a key feature in the progression of osteoporosis, and it makes bones weaker and less able to adapt to changes in physical activity or injury. Medications like bisphosphonates or denosumab aim to restore the balance by inhibiting bone resorption and improving bone density.
10. Increased Risk of Fragility Fractures
A major characteristic of osteoporosis is the heightened risk of fragility fractures. These are fractures that occur from minimal trauma or stress, such as falling from standing height or even coughing or sneezing in severe cases. The most common sites for fragility fractures are the hip, spine, and wrist.
- Impact: Fragility fractures are a clear indication of the weakening of bones and are often the first clinical sign of osteoporosis in patients. They lead to significant morbidity, especially in older adults. For example, hip fractures can lead to long-term disability and a decline in overall quality of life.
- Outcome: Early diagnosis and treatment of osteoporosis can help prevent these fractures, but once they occur, they indicate that the disease is progressing, and more aggressive treatment may be necessary.
11. Vertebral Compression Fractures
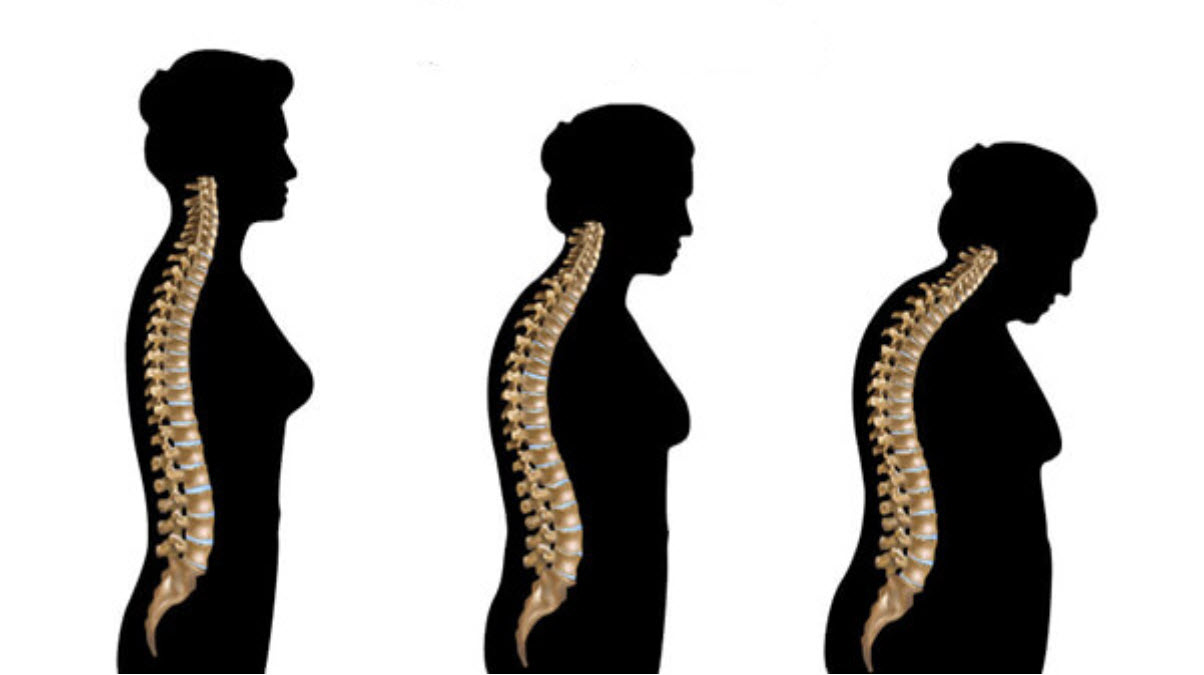
In osteoporosis, the vertebrae are particularly vulnerable to compression fractures. As bone density decreases, the vertebrae can no longer support the weight of the body effectively. Over time, this leads to the collapse of the vertebrae, which often results in spinal deformities like kyphosis (hunched back).
- Impact: Compression fractures can cause back pain, loss of height, and spinal curvature. In severe cases, they can lead to nerve compression or spinal cord injury, which significantly impacts mobility and quality of life.
- Outcome: Vertebral compression fractures are often treated with pain management and physical therapy, but in severe cases, surgical interventions like vertebroplasty or kyphoplasty may be needed.
12. Impaired Bone Quality
While much attention is given to bone density, another important factor in osteoporosis is bone quality. Bone quality refers to the structural properties of bone beyond its density, including its material composition, microdamage accumulation, and tissue-level strength. In osteoporosis, not only does bone mass decrease, but the remaining bone may also be structurally compromised, even if bone density tests suggest only moderate loss.
- Impact: Bone quality impacts the bone’s ability to resist fractures under mechanical load. Even in cases where bone density loss is not severe, poor bone quality can still lead to fractures.
- Outcome: Traditional bone density tests like DEXA (Dual-Energy X-ray Absorptiometry) do not capture bone quality, so individuals with normal or mild bone density loss may still experience fractures if their bone quality is impaired. Emerging technologies like micro-CT scans and biomechanical tests aim to provide a better understanding of bone quality in patients with osteoporosis.
13. Altered Bone Geometry
Another important characteristic of osteoporosis is altered bone geometry, especially in weight-bearing bones like the femur and spine. Changes in bone shape and structure can significantly affect how forces are distributed across bones, making them more susceptible to fractures.
- Impact: As bones lose mass and the structure deteriorates, the geometry of the bone can change. For example, the femoral neck (the region just below the ball of the hip joint) may become thinner or more angled, which increases the risk of a hip fracture.
- Outcome: Altered bone geometry, combined with reduced bone density and quality, leads to a higher likelihood of fractures under normal daily activities, particularly in the elderly. Monitoring these geometric changes can help predict fracture risk more accurately in osteoporotic patients.
14. Bone Mineral Composition Alterations
Bone strength depends on the proper composition and mineralization of bone tissue. In osteoporosis, bone mineral composition may be altered, leading to changes in mineral density and the distribution of hydroxyapatite crystals, which are crucial for bone hardness.
- Impact: Changes in bone mineralization can affect how the bone absorbs impacts and distributes stress. Bones with poor mineral composition may be more brittle and prone to fractures, even if overall bone density seems only mildly reduced.
- Outcome: Understanding mineral composition alterations helps to refine treatment approaches. For example, calcium and vitamin D supplementation is critical in maintaining proper bone mineralization, but other factors, like magnesium and phosphorus, may also play a role.
15. Increased Bone Turnover
In osteoporosis, there is often an increase in bone turnover, which refers to the process by which bone is broken down (resorption) and rebuilt (formation). In healthy bones, these processes are balanced. However, in osteoporosis, bone resorption exceeds bone formation, leading to net bone loss.
- Impact: Increased bone turnover contributes to the thinning of trabeculae and cortical bone. It also results in microstructural damage and an accumulation of microfractures that weaken the bone over time.
- Outcome: Bone turnover markers (BTMs), such as serum C-telopeptide (CTX) and bone-specific alkaline phosphatase (BSAP), can be used to measure the rate of bone resorption and formation. Elevated BTMs are indicative of high bone turnover and may signal a need for anti-resorptive therapies, such as bisphosphonates.
16. Fragility in Non-Weight-Bearing Bones
Although osteoporosis predominantly affects weight-bearing bones like the spine and hip, non-weight-bearing bones can also become fragile in advanced osteoporosis. The ribs and forearms (particularly the radius and ulna) are common sites for fractures in osteoporotic patients, especially after falls or minor traumas.
- Impact: Rib fractures may occur after simple activities like coughing or sneezing. These fractures can be painful and lead to breathing difficulties. Similarly, forearm fractures, such as Colles’ fractures (fractures of the distal radius), are common in osteoporotic individuals who fall and attempt to brace themselves with their hands.
- Outcome: Non-weight-bearing bone fragility highlights that osteoporosis is a systemic disease, affecting multiple bones throughout the body. Preventing falls and addressing overall bone health are crucial in preventing these fractures.
17. Spinal Deformities and Kyphosis
As osteoporosis progresses, multiple vertebral compression fractures can occur, particularly in the thoracic spine. These fractures lead to spinal deformities, including kyphosis (a forward curvature of the upper back, commonly called a dowager’s hump).
- Impact: Kyphosis can cause significant physical and functional impairments, including back pain, difficulty breathing, and digestive issues due to the compression of internal organs. It can also affect balance and mobility, leading to an increased risk of falls and further fractures.
- Outcome: Addressing spinal health in osteoporotic patients is important to prevent severe deformities and maintain quality of life. Treatments may include physical therapy, bracing, and in severe cases, surgical intervention such as vertebroplasty or kyphoplasty.
18. Silent Progression
One of the most challenging aspects of osteoporosis is its silent progression. Many individuals with osteoporosis are unaware of their condition until they suffer a fracture. Unlike conditions that produce noticeable symptoms early on, osteoporosis can progress for years without any obvious signs.
- Impact: The lack of early symptoms means that osteoporosis is often diagnosed only after a fragility fracture occurs. This underscores the importance of early screening, particularly for individuals at high risk, such as postmenopausal women and older adults.
- Outcome: Regular bone density testing (such as DEXA scans) and awareness of risk factors (such as family history, smoking, and sedentary lifestyle) are key in preventing fractures and managing osteoporosis early.
19. Changes in Bone Microenvironment
Osteoporosis does not just affect the bone structure itself; it also changes the microenvironment in which bone cells operate. In healthy bones, there is a balance between osteoclasts (cells that break down bone) and osteoblasts (cells that build new bone). In osteoporosis, this environment becomes more favorable to osteoclast activity, leading to increased bone resorption and reduced formation of new bone.
- Impact: The altered bone microenvironment means that bone turnover is imbalanced, with more bone being lost than produced. This contributes to net bone loss over time and the inability of the bone to repair microdamage effectively.
- Outcome: Therapies like bisphosphonates, denosumab, and teriparatide (a parathyroid hormone analog) target these bone cells to restore balance and improve bone density. Understanding the microenvironment helps to explain why these treatments can slow or reverse bone loss.
20. Sex Hormone Deficiency
Estrogen deficiency in women and testosterone deficiency in men are both critical factors that lead to osteoporosis. Estrogen plays a key role in maintaining bone mass by inhibiting bone resorption, while testosterone has a similar, albeit less pronounced, role in men.
- Impact: After menopause, women experience a rapid decline in estrogen levels, which accelerates bone loss, especially in the first 5-10 years post-menopause. This hormone deficiency is the primary cause of postmenopausal osteoporosis. In men, gradual testosterone decline with aging also leads to increased bone loss, although it tends to occur at a slower rate than in women.
- Outcome: Hormone replacement therapies (HRT) or selective estrogen receptor modulators (SERMs) can help mitigate bone loss in postmenopausal women, while testosterone therapy may be considered for men with clinically significant hypogonadism.
21. Increased Risk of Hip Fractures
One of the most serious consequences of osteoporosis is the increased risk of hip fractures. Hip fractures often occur in the femoral neck or the intertrochanteric region and are more common in older adults due to both bone fragility and increased fall risk.
- Impact: Hip fractures are particularly dangerous because they often require surgery and can lead to long-term disability or even death in elderly individuals. The recovery from a hip fracture is difficult, with many patients losing independence or needing long-term care after the fracture.
- Outcome: Preventing hip fractures is a major focus in osteoporosis management. Strategies include fall prevention, weight-bearing exercises, proper nutrition (especially calcium and vitamin D intake), and bone-strengthening medications.
22. Alterations in Bone Metabolism
In osteoporosis, there are significant alterations in calcium and phosphate metabolism, which are essential for bone health. Calcium is crucial for bone mineralization, and any imbalance in calcium levels can affect bone strength.
- Impact: As bone mass decreases, the body may increase calcium resorption from the bones to maintain blood calcium levels, leading to further weakening of the bone. Similarly, vitamin D deficiency plays a significant role in reducing calcium absorption from the gut, exacerbating osteoporosis.
- Outcome: Calcium and vitamin D supplementation is a foundational part of osteoporosis management. Maintaining proper levels of these nutrients helps slow bone loss and improves bone strength.
23. Impact on Mobility and Quality of Life
Osteoporosis can have a profound impact on a person’s mobility and quality of life, especially as fractures accumulate. Vertebral compression fractures and hip fractures can lead to chronic pain, reduced mobility, and physical deformities like kyphosis (hunched back).
- Impact: These physical changes can severely limit a person’s ability to perform daily activities, leading to loss of independence. Patients may experience chronic pain due to vertebral fractures, difficulty walking, and limitations in bending or lifting.
- Outcome: Reduced mobility can lead to a downward spiral of declining health, as patients become more sedentary and lose muscle mass and balance, increasing their risk of falls and further fractures. Physical therapy and exercise programs designed for people with osteoporosis are critical for maintaining mobility and reducing fall risk.
24. Psychological Impact
The psychological burden of osteoporosis should not be overlooked. The fear of fractures and the limitations on physical activities can lead to anxiety and depression in some patients. The physical deformities that result from spinal compression fractures, such as kyphosis, can also negatively affect self-esteem and body image.
- Impact: Patients with osteoporosis may fear falling or breaking a bone, which can lead them to limit their activities and become more isolated. Chronic pain from fractures also contributes to mood disturbances.
- Outcome: Addressing the psychological impact of osteoporosis is important for overall well-being. Counseling, support groups, and promoting active lifestyles within the patient’s comfort zone can help alleviate these mental health challenges.
25. Silent Fractures and Underdiagnosis
Osteoporosis is sometimes called the “silent disease” because it often progresses without noticeable symptoms until a fracture occurs. Many vertebral compression fractures are silent or asymptomatic, meaning patients may not even realize they have suffered a fracture.
- Impact: Silent fractures can go unnoticed for years, leading to cumulative damage and increased risk of further fractures. This also means that many cases of osteoporosis are underdiagnosed because patients do not seek medical care until they experience a more serious, symptomatic fracture.
- Outcome: Bone density testing (DEXA scans) is critical in detecting osteoporosis before fractures occur. Early diagnosis through regular screenings, especially for high-risk individuals (postmenopausal women, older adults, people with family histories), can help prevent complications by starting treatment sooner.
26. Role of Genetics
Genetic factors play a significant role in determining an individual’s risk of developing osteoporosis. Some people have a family history of the condition, which increases their likelihood of experiencing bone loss and fractures. Certain genetic variations influence bone mineral density, bone remodeling processes, and the overall strength of the skeletal system.
Outcome: Recognizing genetic predisposition can help guide early screening and preventative measures. Genetic testing is not typically part of routine osteoporosis care, but ongoing research is helping to identify specific genes involved in bone health, which may lead to more personalized treatments in the future.
Impact: People with a family history of osteoporosis may be at a higher risk of developing the condition, even if they do not exhibit other risk factors like poor diet or a sedentary lifestyle.

At age 55, the spine maintains a relatively normal posture. By age 65, minor changes are visible, with a slight forward tilt and early signs of vertebral compression. By age 75, the individual shows a significant reduction in spinal height due to multiple vertebral compression fractures, which cause a noticeable forward curve (kyphosis). This change is also accompanied by a decrease in overall height and an altered posture.
These changes illustrate the long-term effects of osteoporosis on the spine, leading to height loss, deformities, and increased susceptibility to fractures, particularly in older adults.
In conclusion, osteoporosis alters bone structure in complex ways, highlighting the importance of early vigilance to prevent serious complications associated with this condition. Understanding the dynamics of bone formation, bone composition and the consequences of the imbalance between resorption and formation offers clear perspectives to guide prevention and treatment strategies, aimed at maintaining bone health throughout life.
Osteoporosis in women
For women, bone loss is most rapid during the first years after adolescence, and it continues until menopause because their ovaries no longer produce estrogen, which helps maintain bone mass. Osteoporosis is more likely to develop if you have not achieved optimal peak bone mass during your bone-building years.
Risk factors
Unchangeable risks
- Sex . Your chances of developing osteoporosis are greater if you are a woman. Women have less bone tissue and lose bone more quickly than men due to changes that occur with menopause.
- Age. The older you are, the higher your risk of osteoporosis. Your bones get thinner and weaker as you age.
- Body size . Small, thin-boned women are at greater risk.
- Ethnicity. White and Asian women are most at risk. African American and Hispanic women have a lower, but significant, risk.
- Family history . The risk of fracture may be due, in part, to heredity. People whose parents have a history of fractures also appear to have reduced bone mass and may be at risk for fractures.
Changeable risks
- Sex hormones . Abnormal absence of menstrual periods (amenorrhea), low estrogen levels (menopause), and low testosterone levels in men can cause osteoporosis.
- Anorexia nervosa. Characterized by an irrational fear of weight gain, this eating disorder increases your risk of osteoporosis.
- Calcium and vitamin D intake . A lifelong diet low in calcium and vitamin D makes you more prone to bone loss.
- Use of medications. Long-term use of certain medications, such as glucocorticoids and some anticonvulsants, can lead to loss of bone density and fractures.
- Way of life. An inactive lifestyle or prolonged bed rest tends to weaken bones.
- Smoking. Smoking is bad for your bones as well as your heart and lungs.
- Alcohol consumption. Excessive alcohol consumption increases the risk of bone loss and fractures.
Classification of osteoporosis
Osteoporosis is a condition characterized by decreased bone density and deterioration of bone tissue, which leads to an increased risk of fractures. It can be classified into various categories based on its causes, affected populations, and underlying mechanisms. Each classification helps in understanding the different ways osteoporosis can present and guides treatment strategies accordingly. Below is a detailed classification of osteoporosis.
1. Primary Osteoporosis
Primary osteoporosis is the most common form of the disease and is typically associated with aging and hormonal changes. It can be further classified into two types:
- Type I (Postmenopausal Osteoporosis): This type of osteoporosis primarily affects postmenopausal women and is linked to the sharp decline in estrogen levels after menopause. Estrogen helps maintain bone density by reducing the rate of bone resorption. In postmenopausal women, the rapid loss of estrogen leads to increased bone breakdown, particularly affecting trabecular bone, which is found in areas like the spine, hip, and wrist. As a result, vertebral compression fractures and wrist fractures (Colles’ fractures) are common in postmenopausal osteoporosis.
- Type II (Senile Osteoporosis): Also known as age-related osteoporosis, this type affects both men and women typically after the age of 70. It involves a more gradual loss of both cortical and trabecular bone and is related to the natural aging process. As people age, bone resorption outpaces bone formation, leading to a slow but steady loss of bone mass. Hip fractures and vertebral fractures are common in senile osteoporosis, and the condition is often compounded by factors like reduced physical activity, poor nutrition, and impaired calcium absorption.
2. Secondary Osteoporosis
Secondary osteoporosis is caused by other medical conditions or external factors that interfere with normal bone metabolism. It affects both men and women of all ages.
- Endocrine Disorders: Diseases like hyperthyroidism, hyperparathyroidism, Cushing’s syndrome, and diabetes can contribute to excessive bone resorption or inadequate bone formation, leading to osteoporosis.
- Medications: Long-term use of glucocorticoids (steroids), anticonvulsants, proton pump inhibitors, and chemotherapy drugs are common causes of secondary osteoporosis. Glucocorticoid-induced osteoporosis is one of the most prevalent forms of secondary osteoporosis and is associated with reduced bone formation and increased bone resorption.
- Malnutrition and Malabsorption: Conditions such as celiac disease, Crohn’s disease, and gastric bypass surgery can lead to deficiencies in calcium and vitamin D, which are crucial for maintaining bone health.
- Chronic Kidney Disease: Kidney dysfunction leads to altered calcium and phosphate metabolism, resulting in renal osteodystrophy, a condition that often contributes to secondary osteoporosis.
- Chronic Inflammatory Conditions: Rheumatoid arthritis, lupus, and chronic infections can cause bone loss either directly through inflammation or indirectly through the use of medications like glucocorticoids.
- Lifestyle Factors: Excessive alcohol intake, smoking, and a sedentary lifestyle all contribute to bone loss, further exacerbating the risk of osteoporosis.
3. Idiopathic Osteoporosis
Idiopathic osteoporosis occurs in otherwise healthy individuals without any identifiable secondary causes. It can affect both young men and women, typically under the age of 50, and even children, in which case it is known as juvenile idiopathic osteoporosis. In these patients, there is a loss of bone density for reasons that remain unclear, though it may be influenced by genetic factors. This type of osteoporosis is relatively rare and can result in fractures, bone pain, and other complications despite the absence of typical risk factors.
4. Localized Osteoporosis
Localized osteoporosis refers to osteoporosis that is restricted to a specific area of the skeleton rather than being generalized. It can occur due to several factors, including disuse, trauma, or repetitive stress on a particular region of the body.
- Disuse Osteoporosis: Immobilization or lack of movement in a specific body part for an extended period can lead to disuse osteoporosis. This can happen after a bone is placed in a cast or splint, or in patients who are bedridden or paralyzed. The lack of mechanical stress on the bone results in a localized loss of bone density. This type of osteoporosis is often reversible once normal movement is restored, with physical therapy and weight-bearing exercises helping to rebuild bone density.
- Trauma-Induced Osteoporosis: Injury to a specific part of the body can lead to localized bone loss. Fractures, especially if severe or if healing is prolonged, can cause osteoporosis in the region around the injury due to a combination of disuse and inflammation.
- Repetitive Local Steroid Injections: Repeated injections of corticosteroids into joints or soft tissues can cause localized osteoporosis. Steroids reduce inflammation but also inhibit bone formation and increase bone resorption. This can lead to the weakening of bones in the injected region, making them more susceptible to fractures and other complications.
- Complex Regional Pain Syndrome (CRPS): Formerly known as reflex sympathetic dystrophy, this syndrome is associated with localized osteoporosis in areas that have experienced trauma or prolonged inflammation. In CRPS, bone loss is typically seen in the affected limb due to a combination of disuse, increased blood flow, and altered autonomic regulation of the area.
Localized osteoporosis is typically managed by addressing the underlying cause, such as reintroducing movement after disuse or modifying the treatment plan to reduce the frequency of local steroid injections. In many cases, the bone loss is reversible with appropriate interventions.
5. Juvenile Osteoporosis
Juvenile osteoporosis is a rare condition that affects children and adolescents, usually between the ages of 8 and 14. It is most often idiopathic, meaning the exact cause is unknown. In some cases, juvenile osteoporosis resolves spontaneously after puberty. However, during its active phase, children may experience bone pain, fractures, and growth disturbances. Early diagnosis and management are critical to avoid permanent skeletal deformities and other long-term complications.
Prevention
To achieve optimal peak bone mass and continue to build new bone tissue as you age, you need to consider several factors.
Calcium
- Insufficient calcium intake over a lifetime can contribute to the development of osteoporosis.
- Many published studies show that low calcium intake appears to be associated with low bone mass, rapid bone loss, and high fracture rates.
- National nutrition surveys show that many people consume less than half the recommended amount of calcium to build and maintain healthy bones.
- Food sources of calcium include low-fat dairy products, such as milk, yogurt, cheese and ice cream; dark green leafy vegetables, such as broccoli, collard greens, bok choy and spinach; sardines and salmon on the bone; Tofu; almonds; and foods fortified with calcium, such as orange juice, cereals and bread.
- Depending on how much calcium you get from food each day, you may need to take a calcium supplement.
Recommended calcium intake
- The body’s demand for calcium is greatest during childhood and adolescence, when the skeleton is developing rapidly, as well as during pregnancy and breastfeeding.
- Postmenopausal women and older men also need to consume more calcium.
- Additionally, as you age, your body becomes less efficient at absorbing calcium and other nutrients. Older adults are also more likely to have chronic health conditions and use medications that can impair calcium absorption.
| Group at life stage | mg/day |
| Infants 0 to 6 months | 200 |
| Infants 6 to 12 months | 260 |
| 1 to 3 years | 700 |
| 4 to 8 years | 1000 |
| 9 to 13 years old | 1300 |
| 14 to 18 years old | 1300 |
| 19 to 30 years old | 1000 |
| 31 to 50 years old | 1000 |
| Men aged 51 to 70 | 1000 |
| Women aged 51 to 70 | 1200 |
| 70 years | 1200 |
| 14 to 18 years old, pregnant/nursing | 1300 |
| 19 to 50 years old, pregnant/nursing | 1000 |
Source: Food and Nutrition Board, Institute of Medicine, National Academy of Sciences, 2010.
Factors helping increase calcium deposition in bone
- Adequate Calcium Intake: A diet rich in calcium is essential for the deposition of calcium in bones. Dairy products, green leafy vegetables, dried fruits and other food sources rich in calcium help support bone mineralization.
- Adequate Vitamin D Intake: Vitamin D is essential for the efficient absorption of calcium from the intestine. Proper exposure to sunlight and a diet that includes sources of vitamin D, such as oily fish, eggs, and fortified products, promotes calcium deposition in bones.
- Physical exercise: Exercise, particularly body-weight bearing activities such as walking, running, and weight training, stimulates bone mineralization by increasing bone mineral density. Exercise also helps strengthen bones and maintain their health.
- Hormones: Certain hormones, such as estradiol (a form of estrogen), promote the deposition of calcium in bones. These hormones play an important role in regulating bone metabolism.
- Hormonal Balance: Overall hormonal balance, including normal levels of parathyroid hormone and calcitonin, is crucial for proper bone metabolism and calcium deposition.
- Nutrients such as vitamin K and magnesium: Vitamin K and magnesium are also involved in bone metabolism. Vitamin K participates in the regulation of proteins that modulate calcium deposition in bones, while magnesium is an essential cofactor in several enzymatic reactions linked to bone formation.
- Healthy body weight: Maintaining a healthy body weight helps reduce the load on bones and promote optimal metabolic balance for calcium deposition
Symptoms of osteoporosis
- Frequent fractures: Osteoporosis makes bones fragile, increasing the risk of fractures. Fractures can occur more easily, even in the absence of major trauma.
- Bone pain: Some individuals may experience pain in their bones, particularly in the back or hips. However, osteoporosis is often asymptomatic until a fracture occurs.
- Loss of height: Repeated vertebral fractures can lead to decreased height and a hunched posture, which may be observed as a loss of height over time.
- Kyphosis (curvature of the spine): Vertebral fractures can contribute to an abnormal curvature of the spine, called kyphosis. This can result in a hunched appearance.
- Loss of muscle mass: Decreased bone density may also be associated with loss of muscle mass, which can contribute to decreased strength and mobility.
- Weakening of the teeth: Osteoporosis can also affect the jaw, leading to weakening of the bones that support the teeth.
Logical Pathway to Osteoporosis Diagnosis
Since osteoporosis is often asymptomatic until a fracture occurs, a logical diagnostic pathway involves risk assessment, clinical evaluation, imaging, and laboratory tests. This structured approach ensures early detection, appropriate management, and prevention of fractures.
Logical Pathway to Osteoporosis Diagnosis
1. Risk Assessment
The initial step in diagnosing osteoporosis involves assessing the patient’s risk factors. Osteoporosis is more common in postmenopausal women and elderly men, but it can affect individuals of any age, particularly those with certain risk factors. A comprehensive review of medical history and lifestyle factors helps identify patients at risk. Key risk factors include:
- Age: Bone density decreases with age, particularly after age 50.
- Sex: Women, especially postmenopausal women, are at higher risk due to the decline in estrogen levels, which accelerates bone loss.
- Family history: A family history of osteoporosis or fragility fractures increases the likelihood of developing the condition.
- Lifestyle factors: Smoking, excessive alcohol consumption, sedentary lifestyle, and poor nutrition (particularly low calcium and vitamin D intake) are contributing factors.
- Medical conditions: Certain conditions, such as rheumatoid arthritis, hyperthyroidism, chronic kidney disease, and celiac disease, predispose individuals to osteoporosis.
- Medications: Long-term use of corticosteroids, anticonvulsants, and certain chemotherapy drugs can lead to bone loss.
After reviewing risk factors, clinicians often use tools like the FRAX score to estimate the 10-year risk of hip or major osteoporotic fractures. The FRAX tool integrates clinical risk factors with or without bone mineral density (BMD) measurements to guide further testing and management decisions.
2. Clinical Evaluation
Although osteoporosis itself typically does not cause symptoms, the presence of fragility fractures (fractures resulting from minimal trauma) raises the suspicion of the disease. Patients with vertebral compression fractures may report back pain, height loss, or kyphosis (curved spine), indicating a possible consequence of osteoporosis.
During the clinical evaluation, the following are assessed:
- Height and posture: Significant height loss (more than 2 cm) may indicate vertebral compression fractures.
- Bone pain: While osteoporosis is often painless, fractures can cause localized pain, particularly in the spine, hips, or wrists.
- Mobility and balance: Reduced mobility or poor balance increases the risk of falls and subsequent fractures.
In some cases, clinicians may identify secondary osteoporosis, which arises from underlying medical conditions or medications that contribute to bone loss. Identifying and managing these causes is essential to prevent further bone deterioration.
3. Bone Mineral Density Testing
The gold standard for diagnosing osteoporosis is the measurement of bone mineral density (BMD) using dual-energy X-ray absorptiometry (DEXA or DXA) scans. DXA is a non-invasive and painless test that measures bone density at the hip, spine, and sometimes the wrist. BMD results are reported as T-scores, which compare the patient’s bone density to that of a healthy young adult:
- Normal: T-score greater than -1.0.
- Osteopenia (low bone mass): T-score between -1.0 and -2.5.
- Osteoporosis: T-score less than or equal to -2.5.
A Z-score is used in premenopausal women, men under 50, and children, comparing bone density to age-matched controls. A Z-score of -2.0 or lower may indicate secondary osteoporosis and warrants further investigation.
4. Laboratory Investigations
To rule out secondary causes of osteoporosis and assess bone health, various laboratory tests may be performed:
- Serum calcium, phosphate, and alkaline phosphatase: These help assess bone metabolism. Abnormalities may suggest conditions like hyperparathyroidism or osteomalacia.
- Vitamin D levels: Vitamin D is crucial for calcium absorption and bone health. Deficiency can exacerbate bone loss.
- Thyroid function tests: Hyperthyroidism can accelerate bone turnover and lead to osteoporosis.
- Parathyroid hormone (PTH): Elevated PTH levels, as seen in hyperparathyroidism, can cause bone resorption and contribute to osteoporosis.
- Renal function tests: Chronic kidney disease can impair bone mineralization and should be evaluated in patients with suspected osteoporosis.
- Markers of bone turnover: Tests like serum C-telopeptide (CTX) and bone-specific alkaline phosphatase can provide insight into the rate of bone formation and resorption.
5. Imaging Studies
While DXA is the primary tool for diagnosing osteoporosis, other imaging modalities may be used in specific circumstances:
MRI or CT scans: These may be used to evaluate complicated cases, such as suspected fractures that are not visible on X-ray.
X-rays: X-rays can identify fractures, vertebral deformities, or other bone abnormalities. However, they are less sensitive than DXA for detecting early bone loss.
Treat osteoporosis
- A comprehensive osteoporosis treatment program emphasizes good nutrition, exercise and safety concerns to prevent falls that can lead to fractures.
Nutrition: The foods we eat contain a variety of vitamins, minerals and other important nutrients that help keep our bodies healthy. All these nutrients are needed in balanced proportion. In particular, calcium and vitamin D are necessary for strong bones and for your heart, muscles and nerves to function properly. (See the “Prevention” section for recommended amounts of calcium.)
Exercise: Exercise is an important part of an osteoporosis prevention and treatment program. Exercise not only improves your bone health, but it increases muscle strength, coordination and balance, and leads to better overall health. Although exercise is good for someone with osteoporosis, it should not put sudden or excessive strain on your bones. As added insurance against fractures, your doctor may recommend specific exercises to strengthen and support your back.
Therapeutic medications: Several medications are available for the prevention and/or treatment of osteoporosis, including: bisphosphonates, calcitonin, estrogen (hormone therapy); estrogen agonists/antagonists (also called selective estrogen receptor modulators or SERMs); parathyroid hormone (PTH) analogue; parathyroid hormone-related protein (PTHrp) analogue; RANK Ligand Inhibitor (RANKL); and tissue-selective estrogen complex (TSEC).
Fall Prevention Strategies to Prevent Osteoporosis-Related Fractures
Osteoporosis is a condition characterized by weakened bones, making individuals more prone to fractures, especially in the hip, spine, and wrist. The risk of fractures increases dramatically when an individual with osteoporosis experiences a fall. Therefore, fall prevention is a critical component in managing osteoporosis and reducing the likelihood of fractures. By implementing comprehensive strategies to minimize fall risk, individuals can maintain mobility, independence, and quality of life while reducing the potential for debilitating injuries.
Below are key strategies and recommendations to prevent falls and reduce osteoporosis-related fractures.
1. Home Environment Modifications
The majority of falls occur at home, so making modifications to create a safer living environment is crucial for fall prevention. Simple changes can significantly reduce the risk of accidents.
- Clear walking pathways: Ensure that floors are free from clutter, loose wires, or other tripping hazards. Arrange furniture to allow easy movement.
- Remove throw rugs: Loose rugs can slip, causing falls. If rugs are necessary, secure them with non-slip backing.
- Improve lighting: Poor lighting is a major cause of falls, especially in hallways, staircases, and bathrooms. Install brighter lights, nightlights, or motion-sensitive lights to improve visibility.
- Handrails and grab bars: Installing handrails along staircases and grab bars in the bathroom (near the toilet and shower) provides additional stability and support.
- Non-slip mats: Use non-slip mats in areas prone to water, such as the bathroom and kitchen, to reduce slipping hazards.
2. Footwear and Assistive Devices
Choosing appropriate footwear and utilizing assistive devices can enhance balance and stability, reducing the risk of falls.
- Proper footwear: Wear shoes that fit well and provide adequate support. Shoes with non-slip soles and low heels are recommended to maintain good traction. Avoid walking barefoot or in slippers that lack grip.
- Assistive devices: Individuals with osteoporosis who have impaired mobility or balance may benefit from assistive devices such as canes, walkers, or walking sticks. A healthcare provider can recommend the most appropriate device based on the individual’s needs.
- Orthotic supports: Some individuals may require orthotics to correct foot alignment, providing additional support and improving balance while walking.
3. Exercise and Balance Training
Exercise plays a vital role in strengthening muscles, improving coordination, and enhancing balance, all of which are essential for fall prevention. Weight-bearing exercises and specific balance training can significantly reduce the risk of falls.
- Strength training: Regular strength training, particularly targeting the lower body (legs, hips, and core muscles), helps improve stability and mobility. Strong muscles provide better support for the bones and improve balance during daily activities.
- Balance exercises: Exercises like tai chi, yoga, and standing on one leg help improve coordination and reduce the likelihood of falls. Balance training can be tailored to an individual’s ability level and can start with simple activities.
- Weight-bearing activities: Exercises like walking, stair climbing, and dancing stimulate bone strength, which can help reduce bone loss in individuals with osteoporosis. These activities improve both bone density and muscle strength, further reducing fall risk.
- Stretching and flexibility: Regular stretching can improve flexibility and reduce joint stiffness, enabling smoother movements and decreasing the chances of losing balance.
4. Medication Review and Management
Certain medications can affect balance, coordination, and overall stability, increasing the risk of falls. A medication review with a healthcare provider can identify potential side effects and adjust medications accordingly.
- Medication side effects: Some medications, such as sedatives, antidepressants, or blood pressure medications, can cause dizziness, lightheadedness, or drowsiness, increasing fall risk. It’s important to consult with a doctor to discuss these side effects and explore alternative treatments if necessary.
- Vitamin D and calcium supplements: Adequate levels of vitamin D and calcium are essential for bone health. Vitamin D aids in calcium absorption and can reduce muscle weakness. A healthcare provider can recommend appropriate supplements to help strengthen bones and reduce fracture risk.
5. Vision and Hearing Care
Vision and hearing impairments contribute to falls by affecting depth perception, balance, and awareness of surroundings. Routine checkups and addressing sensory impairments can significantly reduce fall risk.
- Regular vision exams: Ensure corrective lenses are up to date and regularly monitor vision health. Conditions like cataracts, glaucoma, and macular degeneration can affect depth perception, making falls more likely.
- Hearing aids: Good hearing is important for maintaining balance and spatial awareness. Untreated hearing loss may increase fall risk, so regular hearing tests and the use of hearing aids (if necessary) can help improve stability.
6. Proper Nutrition and Hydration
Nutrition plays an essential role in maintaining bone health and preventing falls. A well-balanced diet supports muscle strength and energy levels, while dehydration can lead to dizziness and fainting, which increase the risk of falling.
- Adequate calcium intake: Calcium is essential for bone health, and low calcium levels can lead to weakened bones and a higher fracture risk. Incorporate calcium-rich foods like dairy products, leafy greens, and fortified cereals into your diet.
- Vitamin D: Ensuring adequate vitamin D levels through diet, supplements, or sunlight exposure is vital for calcium absorption and bone strength.
- Stay hydrated: Dehydration can lead to dizziness, confusion, or fainting, increasing the likelihood of falls. Ensure adequate fluid intake throughout the day, especially for older adults.
7. Regular Health Checkups
Regular visits to healthcare providers for routine checkups can help identify underlying conditions that may contribute to falls. Monitoring conditions like high blood pressure, diabetes, or arthritis allows for timely interventions and management, further reducing fall risk.
Fall prevention is a particular concern for men and women with osteoporosis. Falls can increase the likelihood of breaking a bone in the hip, wrist, spine, or other part of the skeleton. In addition to the environmental factors listed below, falls can also be caused by impaired vision or balance, chronic illnesses that affect mental or physical functioning, and certain medications, such as sedatives and antidepressants. It is important for people with osteoporosis to be aware of any physical changes that affect their balance or gait and to discuss these changes with their health care provider. Here are some tips to help you eliminate the environmental factors that lead to falls.
Vertebral Osteoporosis: Understanding Compression Fractures and Their Consequences
Vertebral osteoporosis is a common form of osteoporosis that particularly affects the spine. It is characterized by a loss of bone density in the vertebrae, making them more susceptible to fractures. One of the most significant and often painful complications of vertebral osteoporosis is compression fractures, which can lead to various structural and functional issues. Below is an overview of the key features associated with vertebral osteoporosis and its complications.
Compression Fractures
Compression fractures are the hallmark of vertebral osteoporosis. These fractures occur when weakened vertebrae can no longer support the body’s weight, leading to a collapse or compression of the vertebral body. The posterior portion of the vertebra is better able to resist vertical compressive forces, so in a compression fracture, the anterior and medial portions are typically more affected, causing them to be crushed while the posterior remains intact. As a result, the vertebra becomes wedge-shaped, where the anterior height is smaller than the posterior height.
A compression fracture may lead to:
- Pain: The fracture site can be extremely painful, with pain varying from acute and sharp to chronic and persistent, depending on the severity and extent of the damage.
- Reduced vertebral height: Compression fractures typically result in a reduction in the height of the affected vertebrae, causing the overall spinal column to shorten. This loss of height is a direct consequence of the structural collapse of the bones.
Importantly, vertebral fractures are often a key predictor of future fractures and should be reported even if they are identified incidentally on radiographs. A vertebral fracture may initially present as simple back pain, which often becomes asymptomatic after 6-8 weeks. However, up to 50% of vertebral fractures can occur in asymptomatic patients, making early detection crucial.
Spinal Deformity
When compression fractures occur repeatedly, they can cause spinal deformities. One of the most common deformities is kyphosis, a forward curvature of the spine, which results in a hunched posture. As multiple vertebrae collapse under the stress of osteoporosis, the spine may curve more severely, leading to visible deformity. This curvature not only affects posture but can also contribute to discomfort and difficulty in performing daily activities.
Spinal Pain
Patients with spinal osteoporosis and compression fractures often experience significant spinal pain. The pain is usually localized to the site of the fracture and may vary in intensity. Acute pain is typically associated with the initial fracture, while chronic pain may develop over time as the spine continues to degenerate and compress. This pain can limit mobility and severely impact the quality of life.
Decreased Body Height
As vertebral fractures accumulate, they contribute to a gradual decrease in body height. This is a common sign of advanced osteoporosis, particularly in older adults. The shortening of the spine due to multiple collapsed vertebrae is a gradual process, and over time, individuals may lose several inches in height. A height loss of more than 5 cm is an indication to perform bone mineral density (BMD) tests and spinal X-rays to assess for osteoporosis and fractures.
Gibbosity (Dorsal Hump) Formation
Severe cases of kyphosis can lead to the formation of a dorsal hump, also known as Dowager’s hump or gibbosity. This hump forms as the spine curves forward dramatically, and the upper back becomes rounded. This deformity not only affects posture but also the aesthetics of the body, giving the appearance of a hunched back. The dorsal hump is often seen in older adults with advanced osteoporosis and can lead to discomfort and difficulty with balance.
Risks of Subsequent Fractures
One of the most concerning aspects of vertebral osteoporosis is the increased risk of subsequent fractures. After sustaining one vertebral compression fracture, the likelihood of having another fracture rises significantly. This increased risk extends beyond the spine, as individuals with spinal osteoporosis are also more prone to fractures in other parts of the skeleton, such as the hip or wrist. This cycle of fractures and weakening bones makes early diagnosis and treatment crucial for preventing further damage.
Radiographic signs of osteoporosis
Osteoporosis is a metabolic bone disease characterized by reduced bone mass and deterioration of bone microarchitecture, which leads to increased bone fragility and susceptibility to fractures. Radiographic evaluation plays a key role in identifying the characteristic features of osteoporosis, particularly through X-ray imaging of the spine and other weight-bearing bones. Several hallmark signs indicate osteoporosis and its complications, particularly in vertebrae, including wedge-shaped vertebrae, picture frame vertebrae, flatfoot vertebrae, and other characteristic deformities. Below is a comprehensive exploration of these radiographic signs associated with osteoporosis.
List of Radiographic Signs
1. Wedge-Shaped Vertebrae (Decreasing Anterior Aspect of the Vertebral Body)
One of the most distinctive radiographic features of osteoporosis is the wedge-shaped vertebra, often resulting from compression fractures. These fractures are a direct consequence of decreased bone density, where the vertebrae can no longer withstand the mechanical forces placed on them, leading to collapse. Wedge-shaped vertebrae develop when the anterior aspect of the vertebral body is more affected than the posterior, creating a wedge-like deformity. This is a hallmark of osteoporosis-related vertebral compression fractures.
Radiographic Signs of Wedge-Shaped Vertebrae:
- Vertebral Collapse: On X-rays, the anterior part of the vertebra appears significantly reduced in height compared to the posterior, giving a wedge-like appearance. The loss of anterior vertebral height is characteristic of compression fractures caused by osteoporosis.
- Widening of the Intervertebral Space: As the anterior portion of the vertebra collapses, the space between adjacent vertebrae can appear widened on radiographs. This widening is often due to the compaction of the fractured vertebra.
- Spinal Deformity: Multiple wedge-shaped vertebrae resulting from repeated compression fractures can lead to kyphosis, a forward curvature of the spine. The deformity progressively worsens with more fractures, contributing to a hunched posture.
- Pain: Though not visible radiographically, vertebral compression fractures often cause pain localized to the area of the fracture. This pain may range from acute to chronic, depending on the severity of the fractures.
2. Picture Frame Vertebrae (Decreased Cortical Bone at the Periphery)
The term picture frame vertebra is used to describe a vertebra that appears to have a thin cortical outline, similar to the edges of a picture frame. In osteoporosis, the cortical bone, which forms the dense outer layer of bones, becomes progressively thinner and weaker. This thinning is particularly noticeable at the periphery of the vertebral body.
Radiographic Signs of Picture Frame Vertebrae:
- Decreased Cortical Bone Density: The cortical bone is visibly thinner on X-rays, especially around the outer edges of the vertebral body. This reduced density is a hallmark of osteoporosis, as the bone becomes more fragile and less resistant to compression.
- Picture Frame Appearance: On X-ray, the thinning cortical bone gives the vertebra a distinctive picture frame-like appearance, with a thinner, weaker perimeter compared to a healthy vertebra. This gives the illusion of a well-defined but hollowed center, much like a picture frame.
- Spinal Compression: Osteoporosis often results in spinal compression fractures, which further reduce the height of the vertebra. This compression, coupled with decreased bone density, accentuates the appearance of the picture frame.
- Spinal Deformities: Like wedge-shaped vertebrae, repeated compression fractures contribute to kyphosis and other spinal deformities. The weakening of the cortical bone makes the spine more susceptible to structural changes over time.
3. Flatfoot Vertebra (Severe Compression Fracture)
In cases of severe osteoporosis, a vertebra may suffer a severe compression fracture, which can give it a characteristic flatfoot appearance on radiographs. This appearance arises when the vertebra loses a significant portion of its height, leading to a flattened shape.
Radiographic Signs of Flatfoot Vertebra:
- Severe Compression Fracture: Due to osteoporosis, the vertebra is highly susceptible to compression. A severe compression fracture can reduce the vertebra to a fraction of its original height, giving it a flatfoot-like appearance on X-rays.
- Flat Upper Surface: The upper surface of the vertebra may appear flattened and enlarged following a severe compression fracture. The flatness is due to the vertebral body’s inability to maintain its structural integrity under mechanical pressure.
- Spinal Deformity: As with other types of compression fractures, multiple flatfoot vertebrae can lead to progressive spinal deformities. Kyphosis or exaggerated forward curvature of the spine is commonly seen in patients with severe osteoporosis.
- Alterations in Vertebral Alignment: Severe compression fractures can cause adjacent vertebrae to become misaligned, leading to altered spinal alignment and contributing to a variety of postural issues.
4. Corner Vertebra
A corner vertebra describes the appearance of a vertebra that has experienced localized compression or collapse at its edges, often due to osteoporosis. This feature is most visible on radiographs and represents a localized area of weakened bone, typically in the corners of the vertebral body.
Radiographic Signs of Corner Vertebra:
- Localized Compression: The corners of the vertebra appear to be compressed or crushed, giving them a flattened or indented appearance. This is a direct result of the bone weakening due to osteoporosis.
- Loss of Height in Specific Areas: Unlike wedge-shaped or flatfoot vertebrae, which affect the entire vertebra, the corner vertebra demonstrates more localized damage, particularly at the corners of the vertebral body.
- Adjacent Vertebral Changes: The compression and alteration of the corner vertebra may cause changes in the adjacent intervertebral spaces, and the alignment of surrounding vertebrae may also be affected, contributing to further spinal deformities.
5. General Signs of Osteoporosis-Related Vertebral Fractures
In addition to specific deformities like wedge-shaped, picture frame, flatfoot, and corner vertebrae, several general radiographic features are commonly associated with osteoporosis-related vertebral fractures:
- Thinning of Cortical Bone: The thinning of the cortical bone around the vertebral body is a hallmark sign of osteoporosis. This thinning makes the bone more susceptible to fractures.
- Trabecular Changes: Osteoporosis also affects the trabecular bone, which is the spongy tissue inside the vertebra. On X-rays, this may appear as a loss of trabecular detail, indicating weakened internal bone structure.
- Reduction in Overall Vertebral Height: As multiple vertebrae collapse due to compression fractures, there is a noticeable reduction in overall spinal height. Patients may lose several inches in height over time, often correlated with the severity of osteoporosis.
- Increased Risk of Fractures in Other Bones: Radiographic findings of osteoporosis in the spine often coincide with weakened bones elsewhere in the body, such as the hips and wrists, increasing the overall risk of fractures.
6. Codfish Vertebra (Biconcave Vertebra)
A codfish vertebra is another deformity seen in osteoporosis, where the vertebrae appear biconcave (concave on both the top and bottom surfaces), resembling the shape of a codfish.
Radiographic Signs of Codfish Vertebra:
- Biconcave Deformity: The endplates of the vertebral bodies become concave due to compression from weakened bones, giving the vertebrae a fish-like appearance on radiographs.
- Central Depression: The central portion of the vertebral body is more affected, with central compression leading to the biconcave shape.
- Seen in Osteoporosis and Osteomalacia: This sign is not exclusive to osteoporosis and can also be seen in conditions like osteomalacia (softening of bones due to vitamin D deficiency). However, in osteoporosis, the deformity typically results from compressive forces on weak trabecular bone.
- Multiple Vertebrae Affected: This deformity often affects multiple vertebrae, contributing to the loss of overall spinal height.
7. Generalized Osteopenia (Diffuse Bone Loss)
Osteopenia refers to the early stages of bone loss, which often precede osteoporosis. On X-ray, osteopenia manifests as generalized bone thinning, and the bones appear more radiolucent (less dense or darker) than normal bones.
Radiographic Signs of Generalized Osteopenia:
- Increased Radiolucency: The bones appear less dense and more transparent than normal on radiographs due to decreased bone mineral content.
- Thinning of the Cortices: The cortical bone, the dense outer layer of the bone, becomes noticeably thinner, particularly in weight-bearing bones like the femur, pelvis, and vertebrae.
- Thinning and Rarefaction of Trabeculae: The trabecular bone, which is the spongy, inner layer of bones, also becomes thinner and more rarefied. This is visible as a loss of trabecular patterns on radiographs.
- Generalized Bone Loss: Osteopenia is often diffuse, affecting multiple bones and joints, but it is particularly noticeable in the spine, hip, and long bones.
8. Trabecular Thinning and Disappearance
In osteoporosis, the trabeculae (the spongy, supporting network within bones) become thinner and may eventually disappear. This is particularly noticeable in the vertebrae and long bones.
Radiographic Signs of Trabecular Thinning:
- Thin and Delicate Trabeculae: On radiographs, the trabeculae may appear thinner and more delicate compared to normal bone structure, indicating early osteoporosis.
- Loss of Horizontal and Vertical Trabeculae: Over time, both the horizontal and vertical trabeculae can thin and may eventually disappear, leaving the bone with only a few remaining struts.
- Haphazard Appearance: As trabeculae disappear, the remaining network becomes more haphazard, with gaps in the normal structure, contributing to the weakened mechanical properties of the bone.
9. Endplate Sclerosis
As a compensatory response to osteoporosis-related vertebral fractures, the endplates of the vertebrae (the superior and inferior surfaces of the vertebral bodies) may become sclerotic (denser) over time.
Radiographic Signs of Endplate Sclerosis:
- Increased Density: On X-ray, the endplates appear denser and more radiopaque (whiter) than the surrounding bone due to the sclerosis of the cortical layer.
- Seen in Vertebral Compression Fractures: Endplate sclerosis is often seen in conjunction with compression fractures, as the bone reacts to increased stress by laying down additional bone tissue at the fracture site.
- Adjacent to Fracture Sites: The sclerosis typically occurs in areas adjacent to the fractured vertebrae, particularly around the superior and inferior endplates.
10. Pelvic Fractures and Sacral Insufficiency Fractures
In addition to vertebral changes, osteoporosis often affects the pelvis and sacrum, leading to insufficiency fractures. These fractures occur with minimal trauma due to weakened bones and are common in postmenopausal women with osteoporosis.
Radiographic Signs of Pelvic and Sacral Insufficiency Fractures:
- Sacral Alar Fracture: Insufficiency fractures often occur in the sacral ala (the wing of the sacrum) and may present as horizontal lines on X-ray or other imaging modalities. These fractures are often missed on standard X-rays and may require CT or MRI for better visualization.
- H-shaped Fracture: A typical insufficiency fracture of the sacrum may appear as an H-shaped pattern on radiographs, especially on CT scans. This pattern is caused by vertical and horizontal fractures through the sacrum.
- Pubic Ramus Fracture: In the pelvis, the pubic rami (the superior and inferior bones of the pelvis) are often involved in insufficiency fractures, which may appear as radiolucent lines across the rami on pelvic X-rays.
11. Thinning of the Iliac Crest
The iliac crest, which forms the uppermost part of the pelvic bone, may show signs of thinning due to osteoporosis. This radiographic sign is often subtle but can contribute to pelvic fragility.
Radiographic Signs of Iliac Crest Thinning:
- Thin Cortical Bone: The cortical bone of the iliac crest may appear thin and more radiolucent on pelvic radiographs, particularly in elderly patients with osteoporosis.
- Increased Risk of Fracture: Thinning of the iliac crest increases the risk of pelvic fractures, especially in patients who have had multiple falls or other trauma.
12. Loss of Horizontal Trabeculae in the Proximal Femur
In the proximal femur, osteoporosis leads to characteristic changes in the trabecular structure, particularly in the greater trochanter and femoral neck. Loss of horizontal trabeculae in this region increases the risk of hip fractures.
Radiographic Signs of Trabecular Loss in the Proximal Femur:
- Disappearance of Horizontal Trabeculae: On X-rays, the horizontal trabeculae in the proximal femur may become thin and eventually disappear, particularly in the greater trochanter and femoral neck.
- Increased Fracture Risk: As the trabeculae thin and disappear, the proximal femur becomes more susceptible to hip fractures, which are common in osteoporotic patients, especially after a fall.
13. Cortex to Medullary Ratio Reduction
In osteoporosis, the cortex to medullary ratio of long bones decreases. This occurs because the cortical bone (the dense outer layer) thins out, and the medullary cavity (the inner, spongy part of the bone) enlarges due to trabecular bone loss.
Radiographic Signs of Cortex to Medullary Ratio Reduction:
- Thinning of Cortical Bone: The cortical bone becomes thinner and more radiolucent (darker) on X-rays, especially in the long bones like the femur, tibia, and humerus.
- Widening of Medullary Cavity: The medullary cavity enlarges, resulting in a lower cortex to medullary ratio. This change is most noticeable in weight-bearing bones.
- Generalized Bone Loss: This sign often presents alongside generalized osteopenia, where the entire skeleton appears to have lost density.
14. Pencil-Thin Cortices
A term commonly used to describe severe cortical thinning seen in long bones is pencil-thin cortices. This finding is especially noticeable in patients with advanced osteoporosis.
Radiographic Signs of Pencil-Thin Cortices:
- Thin, Radiolucent Cortices: The cortical bone appears almost pencil-thin on radiographs, particularly in long bones such as the radius, ulna, tibia, and femur.
- Increased Fracture Risk: The extremely thin cortices make the bones highly prone to fractures, even with minimal trauma.
- Uniformly Thinned Cortices: This thinning tends to be uniform along the shaft of long bones, as opposed to more focal thinning seen in some other bone diseases.
15. Looser’s Zones (Pseudofractures)
Looser’s zones, also known as pseudofractures, are radiographic signs seen in patients with conditions related to bone demineralization, such as osteomalacia. However, they can also appear in patients with severe osteoporosis, where bone fragility causes stress fractures.
Radiographic Signs of Looser’s Zones:
- Thin Radiolucent Lines: Looser’s zones appear as radiolucent (dark) lines perpendicular to the cortical bone, often in the long bones, ribs, and pelvis.
- Bilateral Symmetry: These pseudofractures are typically bilateral and symmetrical, and they do not extend through the full thickness of the bone.
- Associated with Fragility: While more commonly associated with osteomalacia, Looser’s zones can appear in osteoporotic bones that have undergone repetitive stress, leading to incomplete fractures.
16. Decreased Vertical Striations of the Vertebrae
Another early radiographic sign of osteoporosis is the decrease in vertical striations within the vertebral body. These striations represent the trabeculae, the internal latticework that provides structural support.
Radiographic Signs of Decreased Vertical Striations:
- Loss of Vertical Trabeculae: On radiographs, the internal vertical striations (trabeculae) become less distinct or disappear, indicating a loss of bone strength.
- More Pronounced in Thoracic and Lumbar Spine: This sign is often first noticed in the thoracic and lumbar spine, where the load-bearing trabeculae are crucial for structural integrity.
- Increased Radiolucency: As vertical trabeculae disappear, the vertebral bodies appear more radiolucent, making the bones look weaker and more fragile.
17. Sclerosis of Weight-Bearing Areas
In osteoporosis, the body may respond to bone loss by laying down new bone in weight-bearing areas as a compensatory mechanism. This results in sclerosis (increased bone density) in certain parts of the vertebrae and pelvis.
Radiographic Signs of Sclerosis in Weight-Bearing Areas:
- Increased Density in Endplates: The superior and inferior endplates of the vertebrae may become sclerotic as they bear the increased stress from vertebral body compression.
- Sclerosis in the Sacroiliac Joints: The sacroiliac joints and the pelvic bones may show localized sclerosis, especially where stress and load are concentrated.
- Contrast Between Sclerotic and Osteoporotic Bone: Sclerotic areas will appear more radiopaque (whiter) compared to the adjacent osteoporotic bone, which is radiolucent.
18. Subchondral Sclerosis
Subchondral sclerosis refers to the hardening of the bone just beneath the cartilage surface. While this finding is often associated with osteoarthritis, it can also be present in osteoporotic bones that undergo microfractures and reactive bone formation.
Radiographic Signs of Subchondral Sclerosis:
- Increased Bone Density Beneath Joint Surfaces: On X-rays, the bone just beneath the joint surfaces, particularly in the hip and knee joints, may appear denser and more radiopaque.
- Thickened Subchondral Bone: The subchondral bone may become thickened in response to increased stress, a compensatory mechanism in osteoporotic joints.
- Often Associated with Joint Pain: Though not always symptomatic, subchondral sclerosis may contribute to joint pain, particularly in areas where stress is concentrated due to osteoporosis.
19. Fracture of the Proximal Humerus (Shoulder Fracture)
Although not exclusively seen in the spine or pelvis, fractures of the proximal humerus are common in individuals with osteoporosis. These fractures typically occur due to falls and are indicative of fragile bones.
Radiographic Signs of Proximal Humerus Fractures:
- Fracture Lines in the Humeral Neck: On radiographs, the surgical neck of the humerus often shows a fracture line due to a fall on an outstretched hand.
- Displacement or Comminution: Depending on the severity, the fracture may be displaced or show comminution (multiple bone fragments).
- Thin Cortices: The bone surrounding the fracture site often shows signs of cortical thinning, making it more susceptible to fractures.
20. Advanced Imaging Modalities in Osteoporosis Diagnosis
While X-rays are the most commonly used imaging modality for diagnosing osteoporosis and its complications, advanced imaging techniques provide more detailed information about bone density and structural integrity:
Magnetic Resonance Imaging (MRI): MRI is useful in evaluating bone marrow and detecting early vertebral compression fractures that may not be visible on X-ray. It also helps in assessing avascular necrosis (AVN) of the femoral head, which is a complication of severe osteoporosis.
Dual-Energy X-ray Absorptiometry (DXA): This is the gold standard for measuring bone mineral density (BMD). DXA scans quantify bone density in the spine, hip, and wrist, helping to confirm the diagnosis of osteoporosis.
Quantitative Computed Tomography (QCT): QCT provides a three-dimensional analysis of bone density, with specific focus on the trabecular bone. This method is highly sensitive in detecting early bone loss in the spine and other areas.
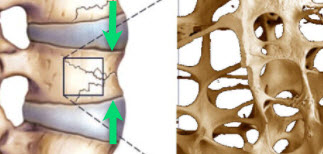
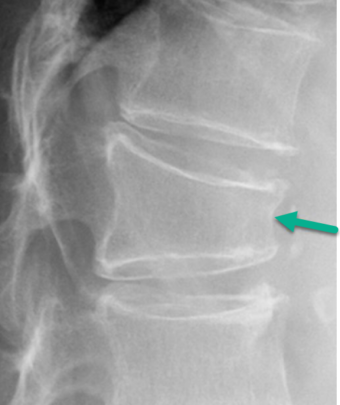
Striation of the vertebrae
Decrease in horizontal trabeculae and increase in vertical trabeculae gives an appearance of striation to the vertebral body.

Picture frame appearance
Due to resorption processes, the vertebral bodies show an overall increase in radiolucency and a thin, well-demarcated cortical margin.
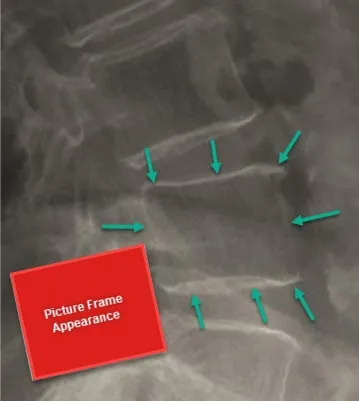
Vertebra shaped like a flat foot
Is the term given when a vertebral body has lost almost all of its height anteriorly and posteriorly, representing a very advanced compression fracture.
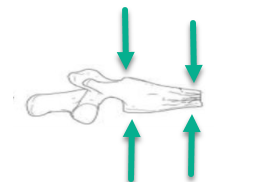

References
- Varacallo MA, Fox EJ. Osteoporosis and its complications. Med Clin North Am. 2014 Jul;98(4):817-31, xii-xiii. [ PubMed ]2.
- Varacallo MA, Fox EJ, Paul EM, Hassenbein SE, Warlow PM. Patients’ response toward an automated orthopedic osteoporosis intervention program. Geriatr Orthop Surg Rehabil. 2013 Sep;4(3):89-98. [ PMC free article ] [ PubMed ]3.
- Varacallo M, Seaman TJ, Jandu JS, Pizzutillo P. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 4, 2023. Osteopenia. [ PubMed ]4.
- Kanis JA, Johansson H, Harvey NC, McCloskey EV. A brief history of FRAX. Arch Osteoporos. 2018 Oct 31;13(1):118. [ PMC free article ] [ PubMed ]5.
- Walzak LC, Loken Thornton W. The role of illness burden in theory of mind performance among older adults. Exp Aging Res. 2018 Oct-Dec;44(5):427-442. [ PubMed ]6.
- Greenstein AS, Gorczyca JT. Orthopedic Surgery and the Geriatric Patient. Clin Geriatr Med. 2019 Feb;35(1):65-92. [ PubMed ]7.
- Varacallo M, Davis DD, Pizzutillo P. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 28, 2023. Osteoporosis in Spinal Cord Injuries. [ PubMed ]8.
- Prince RL, Lewis JR, Lim WH, Wong G, Wilson KE, Khoo BC, Zhu K, Kiel DP, Schousboe JT. Adding Lateral Spine Imaging for Vertebral Fractures to Densitometric Screening: Improving Ascertainment of Patients at High Risk of Incident Osteoporotic Fractures. J Bone Miner Res. 2019 Feb;34(2):282-289. [ PubMed ]9.
- Rachner TD, Hofbauer LC, Göbel A, Tsourdi E. Novel therapies in osteoporosis: PTH-related peptide analogs and inhibitors of sclerostin. J Mol Endocrinol. 2019 Feb 01;62(2):R145-R154. [ PubMed ]10.
- Khadka B, Tiwari ML, Gautam R, Timalsina B, Pathak NP, Kharel K, Sharma S, Acharya D. Correlates of Biochemical Markers of Bone turnover among Post-Menopausal Women. JNMA J Nepal Med Assoc. 2018 Jul-Aug;56(212):754-758. [ PMC free article ] [ PubMed ]11.
- Jiang SY, Kaufman DJ, Chien BY, Longoria M, Shachter R, Bishop JA. Prophylactic Fixation Can Be Cost-effective in Preventing a Contralateral Bisphosphonate-associated Femur Fracture. Clin Orthop Relat Res. 2019 Mar;477(3):480-490. [ PMC free article ] [ PubMed ]12.
- Larsen MS, Schmal H. The enigma of atypical femoral fractures: A summary of current knowledge. EFORT Open Rev. 2018 Sep;3(9):494-500. [ PMC free article ] [ PubMed ]13.
- Lewiecki EM. New and emerging concepts in the use of denosumab for the treatment of osteoporsis. Ther Adv Musculoskelet Dis. 2018 Nov;10(11):209-223. [ PMC free article ] [ PubMed ]14.
- Capdevila-Reniu A, Navarro-López M, López-Soto A. Osteoporotic vertebral fractures: A diagnostic challenge in the 21st century . Rev Clin Esp (Barc). 2021 Feb;221(2):118-124. [ PubMed ]15.
- Lopez-Olivo MA, des Bordes JKA, Syed MN, Alemam A, Dodeja A, Abdel-Wahab N, Suarez-Almazor ME. Quality appraisal of educational websites about osteoporosis and bone health. Arch Osteoporos. 2021 Feb 10;16(1):28. [ PubMed ]