Pronator teres syndrome (PRS), first described by Henrik Seyffarth in 1951, is caused by compression of the median nerve (MN) by the pronator teres (PR) muscle of the forearm. The PR muscle is named for its action and shape; it is a rounded muscle that performs the pronation movement.
Introduction
The introduction to a topic as vast and complex as Pronator Teres Syndrome in the context of osteopathy requires a clear and informative orientation. Here is a general introduction that you could use:
Pronator Teres Syndrome represents a common orthopedic challenge characterized by elbow pain and mobility limitations. In the field of osteopathy, the approach to this syndrome goes beyond simple symptom management, extending to a thorough understanding of the underlying mechanisms, nervous system influences, and implications for musculoskeletal health.
This review explores the various facets of Pronator Teres Syndrome from an osteopathic perspective, highlighting diagnostic techniques, alternative treatment approaches, and considerations specific to the pediatric population. By examining the links between muscle imbalances, myofascial tensions, and nervous system interactions, we seek to uncover the holistic approach that distinguishes osteopathy in the management of this syndrome.
Through this detailed exploration, we will discover how osteopathy personalizes care for each patient, striving not only to relieve immediate symptoms but also to restore musculoskeletal balance in the long term. By incorporating pediatric perspectives, this study offers insight into the specific considerations of children, emphasizing the importance of an approach tailored to their unique growth and development.
Let’s dive into this in-depth look at Pronator Teres Syndrome through the lens of osteopathy, highlighting the techniques, principles, and implications for comprehensive management of this orthopedic condition.
Understanding Pronator Teres Syndrome
- Elbow Pain: People with Pronator Teres Syndrome typically experience persistent pain in the elbow, especially when flexing or extending the joint.
- Joint Stiffness: Stiffness may develop, limiting the range of motion of the elbow. This may be particularly noticeable during full extension or flexion of the arm.
- Muscle Weakness: The condition can cause muscle weakness in the elbow area, affecting the ability to perform simple movements and causing early fatigue of the muscles.
- Abnormal Sensations: Some individuals may experience abnormal sensations such as tingling, numbness, or burning sensations in the elbow area.
- Trigger Points: Trigger points, which are hypersensitive areas in the muscles, can form and contribute to muscle pain and tension.
Causes of Pronator Teres Syndrome
Pronator Teres Syndrome is a compression neuropathy of the median nerve as it passes between the heads of the pronator teres muscle in the forearm. This condition can result in forearm pain and sensory disturbances in the median nerve distribution of the hand. Here are some of the primary causes of Pronator Teres Syndrome:
List of Causes:
- Repetitive Movements:
- Frequent Pronation: Activities that require repetitive pronation of the forearm, such as typing, using a screwdriver, or playing racquet sports, can lead to overuse of the pronator teres muscle.
- Forceful Gripping: Repeated gripping or grasping motions can also contribute to increased pressure on the median nerve.
- Muscle Hypertrophy:
- Increased Muscle Size: Athletes or individuals who perform activities that lead to the hypertrophy of the pronator teres muscle may experience compression of the median nerve due to the reduced space between muscle fibers.
- Direct Trauma:
- Injury: Direct trauma or a blow to the forearm can cause swelling or bruising of the pronator teres muscle, leading to nerve compression.
- Fractures: A fracture of the forearm bones (radius or ulna) or elbow can lead to altered anatomy, which can compress the median nerve.
- Anatomical Variations:
- Abnormal Muscle Origin: Some individuals may have variations in the anatomical structure of the pronator teres muscle, such as additional fibrous bands that may compress the median nerve.
- Anomalous Struthers’ Ligament: Occasionally, an extra ligament, known as Struthers’ ligament, may cause compression if it extends over the median nerve.
- Inflammation or Swelling:
- Tendinitis or Tenosynovitis: Inflammation of the tendons or synovial sheath around the pronator teres can increase pressure on the median nerve.
- Rheumatoid Arthritis: Inflammatory conditions like rheumatoid arthritis may contribute to swelling in the forearm, compressing the median nerve.
- Occupational Factors:
- Ergonomic Issues: Poor ergonomic setup in the workplace can lead to prolonged positions that stress the forearm muscles and increase the risk of developing the syndrome.
- Vibrational Tools: Use of vibrational tools such as jackhammers can cause repetitive strain on the forearm muscles.
- Fibrous Band Formation:
- Fibrotic Changes: Chronic use or injury can lead to fibrous bands forming within or near the pronator teres, restricting the space for the median nerve.
- Systemic Conditions:
- Diabetes: Patients with diabetes may have an increased risk due to peripheral nerve susceptibilities and potential for nerve compression.
- Tumors or Cysts:
- Space-Occupying Lesions: Rarely, tumors or cysts in the forearm can compress the median nerve, mimicking or contributing to Pronator Teres Syndrome.

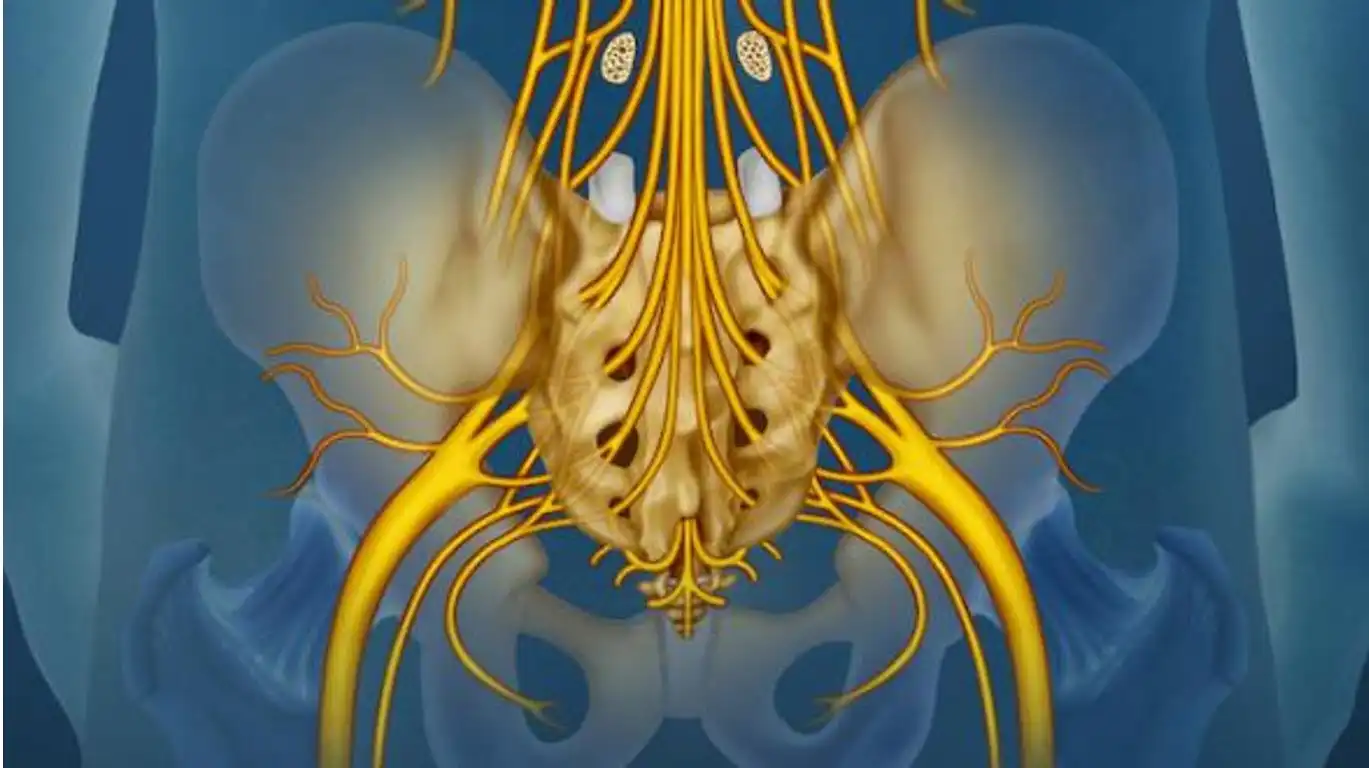
This diagram illustrates the anatomical structures involved in Pronator Teres Syndrome, a condition where the median nerve is compressed as it passes between the humeral head and ulnar head of the pronator teres muscle. The humerus, radius, and ulna bones are labeled to highlight their relationship with the muscles and the median nerve, which can become entrapped, leading to symptoms such as forearm pain and numbness in the hand.
Symptoms
Pronator teres syndrome is characterized by specific symptoms resulting from compression of the median nerve at the elbow. Symptoms can vary from person to person, but they commonly include the following:
- Elbow pain: Pain is a common symptom of pronator teres syndrome and is usually felt in the elbow, often on the inner (medial) side.
- Pain radiating to the hand and fingers: Pain may radiate along the path of the median nerve, causing painful sensations in the hand and fingers, especially the second and third fingers.
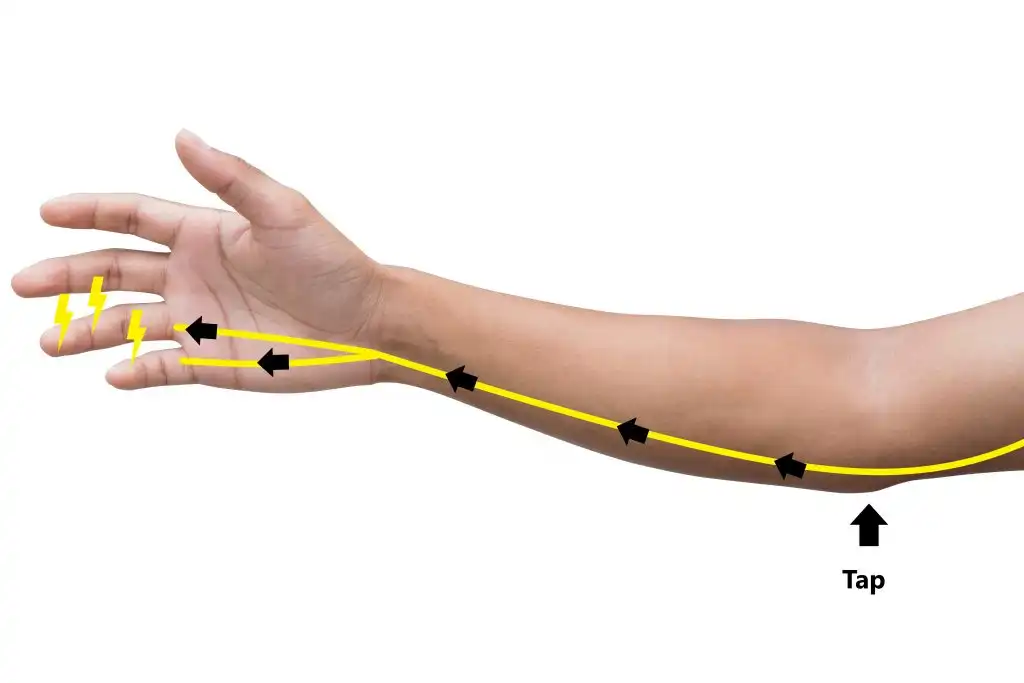
- Numbness and tingling: Numbness and tingling, also called paresthesia, may be felt in areas innervated by the median nerve, usually the palm, fingers, and sometimes the thumb.
- Muscle weakness: Compression of the median nerve can lead to muscle weakness in the hand, particularly in the muscles innervated by this nerve.
- Burning sensations: Some people may experience burning sensations in the hand or fingers.
- Feeling of heaviness: A feeling of heaviness or fatigue in the hand may also be present.
- Difficulty grasping objects: Due to muscle weakness and sensory symptoms, it may be difficult to grasp or hold objects with the affected hand.
Osteopathic Diagnosis and Evaluation of Pronator Teres Syndrome
Osteopathic diagnosis and assessment of Pronator Teres Syndrome involves a holistic approach to understanding the underlying factors that contribute to the condition. Osteopaths use a variety of techniques to assess anatomical structures, joint mobility, posture, and soft tissues. Here is how osteopaths may diagnose and assess Pronator Teres Syndrome, with a focus on the specific techniques used:
- Anamnesis (Interrogation):
- Osteopaths begin by gathering detailed information about the patient’s medical history, lifestyle habits, daily activities, and symptoms. This helps to understand the overall context of the condition.
- Postural Assessment:
- The osteopath observes the patient’s overall posture, particularly the position of the elbow and shoulders. Postural imbalances can provide clues to muscle tension and joint dysfunction.
- Joint Mobility Assessment:
- Palpation techniques are used to assess elbow joint mobility. The osteopath examines flexion, extension, rotation and other movements to identify possible restrictions or blockages.
- Soft Tissue Palpation:
- Using palpation, the osteopath assesses the soft tissues around the elbow, including muscles, tendons and ligaments. Areas of tension, tenderness or trigger points may be identified.
- Neurological Tests:
- Neurological tests may be performed to assess nerve function, particularly if pronator teres syndrome is associated with neurological symptoms such as tingling or numbness.
- Assessment of Vascularization:
- The osteopath can assess blood circulation in the elbow area to detect signs of vascular alterations or inflammation.
- Muscle Function Assessment:
- Muscle strength tests are performed to assess the strength of the muscles surrounding the elbow, thereby identifying any weaknesses or imbalances.
- Evaluation of the Kinetic Chain:
- The osteopath may expand the assessment to include other parts of the body, particularly the kinetic chain associated with the elbow. This may reveal compensations or dysfunctions in other areas of the body.
Osteopathic Treatment of Pronator Teres Syndrome
- Gentle Joint Mobilizations:
- Gentle joint mobilizations aim to improve elbow joint mobility by applying controlled and progressive movements. This can help release tension and restore normal joint function.
- Libération Myofasciale :
- Myofascial release targets tension in the muscles and fascia surrounding the elbow. Techniques may include gentle pressure, stretching, and massage to release tight tissues.
- Trigger Points:
- Identification and deactivation of trigger points, often achieved by ischemic pressure, is commonly used to relieve local pain and muscle tension associated with the syndrome.
- Muscle Strengthening Exercises:
- Targeted muscle strengthening exercises are prescribed to restore strength and balance in the muscles surrounding the elbow. This may include flexion, extension, rotation, and stabilization exercises.
- Stretching:
- Specific stretches are recommended to improve flexibility of the elbow muscles and tendons, thereby reducing tension and stiffness.
- Muscle Relaxation Techniques:
- Techniques to reduce muscle tension, such as progressive relaxation, can be incorporated to help relax affected muscles.
- Postural Tips:
- Osteopaths often provide advice on ergonomics and posture to minimize stress on the elbow in daily activities.
- Patient Education:
- Patient education about contributing factors, pain management, and lifestyle adjustments can play a crucial role in treatment.
Exercises and Self-Massages Recommended by Osteopathy
1. Self-massage with a Tennis Ball:
- Technique: Place a tennis ball on a flat surface. Using your body weight, gently roll the ball under your forearm in a circular motion.
- Purpose: This can help release tension in the arm muscles, including the pronator teres.
2. Wrist and Forearm Stretches:
- Technique :
- Extend your arm in front of you with your palm facing up.
- Use the other hand to gently pull your fingers down.
- Tilt your hand slightly outward to stretch the pronator teres.
- Hold for 15-30 seconds and repeat on the other side.
- Objective: To improve flexibility and reduce tension in the forearm muscles.
3. Resistance Exercises for Elbow Muscles:
- Technique :
- Use a resistance band or elastic band.
- Secure the rubber band around your hands.
- Perform wrist flexion and extension movements while resisting the tension of the elastic.
- Objective: To strengthen the elbow muscles, including the pronator teres.
4. Self-massage of Trigger Points:
- Technique: Use your thumb to apply gentle, targeted pressure to the identified trigger points around the elbow. Hold the pressure for 15-30 seconds and gradually release.
- Purpose: Relieve trigger points and reduce muscle tension.
5. Wrist Rotation Exercises:
- Technique :
- Extend your arm in front of you with your palm facing down.
- Use the other hand to apply light pressure to the back of your hand, creating an inward rotation.
- Objective: To improve mobility and flexibility of the wrist and forearm.
6. Self-Mobilization of the Elbow Joint:
- Technique: Use gentle flexion, extension, and rotation movements to mobilize the elbow joint. Do not force the movements and stay within a comfortable range of motion.
- Objective: To improve joint mobility and reduce stiffness.
It is essential that patients discuss these exercises with their osteopath before incorporating them into their daily routine. A healthcare professional will be able to tailor these recommendations to each individual’s specific needs and provide additional advice on how to relieve the symptoms of Pronator Teres Syndrome.
Pediatric Osteopathic Approach to Pronator Teres Syndrome
The pediatric osteopathic approach to Pronator Teres Syndrome requires careful consideration of the anatomical and physiological particularities of children. Here are some important points to consider when treating this syndrome in children with osteopathic treatment, highlighting the differences compared to adults:
**1. Understanding Musculoskeletal Development:
- Children are constantly growing and developing. Pediatric osteopaths must have a thorough understanding of the stages of musculoskeletal development in children to adapt their techniques accordingly.
**2. Gentle and Adapted Approach:
- Pediatric osteopaths generally favor gentle techniques adapted to the sensitivity of tissues in children. Manipulations are often less intense and more subtle compared to adults.
**3. Use of Games and Playful Techniques:
- Incorporating games and playful techniques can help build trust with the child, promoting effective cooperation during treatment. Children often respond best to approaches that engage them in a positive way.
**4. Incorporation of Gentle Myofascial Techniques:
- Gentle myofascial release techniques are often preferred in children to release muscle tension without causing excessive discomfort. These techniques can be applied to treat the symptoms of Pronator Teres Syndrome.
**5. Adapted Postural Assessment:
- Postural assessment in children takes into account ongoing growth and may require adjustments compared to that of adults. Osteopaths also observe motor behaviors and posture specific to each stage of development.
**6. Global Approach Taking into Account Related Systems:
- Pediatric osteopaths take a holistic approach that considers related systems, including the nervous system, circulatory system, and musculoskeletal system, integrating adjustments based on the child’s individual needs.
**7. Age Appropriate Communication:
- Communication with the child should be adapted to their level of understanding. Osteopaths use simple language and age-appropriate explanations to ensure that the child feels comfortable and understood.
**8. Inclusive Consent:
- Pediatric osteopaths strive to include the child in the treatment process by obtaining their consent whenever possible. This helps to establish a climate of trust and collaboration.
It is essential that parents or guardians are fully informed and involved in the pediatric osteopathic treatment process. Collaboration between the osteopath, child and parents helps ensure appropriate, safe and effective care for the treatment of Pronator Teres Syndrome in children.
Conclusion
In conclusion, the osteopathic approach to Pronator Teres Syndrome is part of a holistic perspective, considering the interconnection of anatomical, physiological and neurological systems. Osteopathy recognizes that this syndrome, characterized by elbow pain and mobility limitations, can result from a variety of factors, including muscular imbalances, myofascial tension, joint restrictions and nervous system influences.
In the osteopathic assessment process, special attention is paid to the different components of the syndrome, ranging from the analysis of anatomical structures to the assessment of neurological responses. Osteopaths use a variety of techniques, such as joint mobilizations, myofascial release, gentle manipulations, and personalized advice on posture and exercises.
Pediatric osteopathy brings a specific dimension to the treatment of Pronator Teres Syndrome in children, taking into account the particularities of musculoskeletal development and adopting approaches adapted to their sensitivity.
With an emphasis on personalized care, osteopathy aims to restore musculoskeletal balance, improve joint mobility and relieve symptoms associated with the syndrome. Patients are also educated on preventative aspects and how to integrate lifestyle habits that support musculoskeletal health.
It is important to emphasize that osteopathic treatment of Pronator Teres Syndrome should be performed by qualified health professionals, after a thorough assessment and in collaboration with other health professionals as needed. Each treatment plan is tailored to the individual needs of the patient, thus promoting lasting results and an improvement in quality of life.
References
- Greenman, P. E. (1996). Principles of Manual Medicine. Lippincott Williams & Wilkins.
- Chaitow, L. (2003). Cranial manipulation: Theory and practice. Elsevier Health Sciences.
- DiGiovanna, E. L., & Schiowitz, S. (2005). An Osteopathic Approach to Diagnosis and Treatment. Lippincott Williams & Wilkins.
- Hanten, W. P., Chandler, S. D., & Raczynski, J. M. (1990). Manipulative therapy for upper extremity pain and dysfunction: a systematic review. Journal of Manual & Manipulative Therapy, 4(4), 151-159.
- Cerritelli, F., Chiacchiaretta, P., Gambi, F., Ferretti, A., & Vanacore, N. (2015). Osteopathy for primary headache patients: a systematic review. The journal of headache and pain, 16(1), 1-12.
- Licciardone, J. C., Kearns, C. M., Hodge, L. M., & Bergamini, M. V. W. (2012). Associations of cytokine concentrations with key osteopathic lesions and clinical outcomes in patients with nonspecific chronic low back pain: Results from the OSTEOPATHIC Trial. The Journal of the American Osteopathic Association, 112(9), 596-605.