Rheumatoid arthritis (RA) is a disease in which the immune system decides to attack the human cell instead of the foreign one. In the joint, it is the surface of the interior synovial membrane that is targeted.
Introduction
The active attack of the inflammatory system in joint disorders, such as rheumatoid arthritis (RA), generates devastating consequences in the joints and soft tissues. This inflammatory process triggers a characteristic swelling of the spindle-shaped soft tissues, creating a chain response that can lead to juxta-articular osteoporosis. What makes this inflammation unique is its ability to break down cartilage and bone, leading to a gradual loss of these crucial structures.
The resulting loss of cartilage and bone can lead to joint misalignment, causing uniform narrowing of the joint space. This degradation can be severe, leading to erosions at the joint margins, often referred to as “bare areas”. This phenomenon is characterized by irreversible damage which, in many cases, shows no capacity for natural repair. When cartilage is entirely removed from the joint surfaces, it becomes possible for these surfaces to fuse, leading to what is known as joint ankylosis .
Rheumatoid arthritis, a chronic inflammatory disorder, has a still unknown etiology, making its treatment and management complex. This condition primarily targets synovial joints and initially manifests in small peripheral joints. Characteristically, it often progresses symmetrically and can progress to affect proximal joints. The duration of symptoms is a key factor in categorizing RA, being classified as early when symptoms have persisted for less than six months and established when they have been present for more than six months.
The heart of the problem lies in the immune system’s attack on the tissues that cushion and line the joints. In a mechanism that is still poorly understood, white cells of the immune system view the joint capsule, also known as the synovial membrane, as a foreign body and target it aggressively. This persistent attack leads to joint pain, progressive loss of mobility and, ultimately, destruction of the affected joints.
In short, understanding the complex mechanisms underlying rheumatoid arthritis makes it possible to understand the devastating consequences of this autoimmune disease on the joints. Ongoing research aims to further elucidate the root causes of this condition, paving the way for more targeted treatment approaches and more effective preventative interventions. Meanwhile, management of rheumatoid arthritis focuses on reducing inflammation, relieving symptoms, and preserving joint function to improve the quality of life of those affected.
Joints affected by rheumatoid arthritis
The joints most commonly affected by rheumatoid arthritis include:
- Small joints of the hands and feet: The joints of the fingers, hands, wrists, as well as the joints of the toes and feet are often affected. Rheumatoid arthritis tends to affect symmetrically, meaning it usually affects the same joints on both sides of the body.
- Wrists: The wrists are frequently affected, leading to stiffness and limited mobility.
- Elbows: The elbow joints can also be affected, causing pain and swelling.
- Shoulders: The shoulders may be affected, which can lead to decreased mobility and muscle strength.
- Knees: The knees are often involved in rheumatoid arthritis, leading to inflammation, pain and stiffness.
- Ankles: The ankles may be affected, which can affect walking and stability.
- Hips: Although less commonly than other joints, the hips can also be affected, causing pain and stiffness.
- Spine: In some cases, rheumatoid arthritis can also affect the joints of the spine, especially those in the neck, which can lead to stiffness and difficulty moving.
Stage of attack on the synovial membrane by the immune system
- The attacked membrane becomes inflamed and painful, the entire joint capsule begins to swell, and the synovial cells begin to grow and divide abnormally.
- Almost as if triggering a counterattack, these abnormal cells invade the surrounding tissues, particularly the bone and cartilage of the affected joint.
- The joint space decreases and the support structures of the joint become weak. At the same time, the cells that started the inflammation produce enzymes that attack the bone and cartilage, causing erosion and scarring of the joint.
- Under the effect of this multiple attack, the joint itself deteriorates and ends up deforming and becoming misaligned.
RA symptoms
- Ear pain, warmth, redness, swelling or tension
- Swelling of three or more joints for six weeks or more.
- The same symptoms on both sides of the body (for example, both hands or both knees).
- Weightloss.
- Fever.
- Fatigue or weariness.
- Weakness.
- Joint pain or stiffness lasting more than an hour upon getting up or after prolonged inactivity.
- Subcutaneous bump (rheumatoid nodule), especially on pressure points like the elbows or feet.
Risk factors
- Family history : Some people have specific genes that develop RA. However, having RA-related genes does not necessarily mean developing RA.
- Gender : RA affects women two to three times more often than men.
- Hormones : Certain hormonal changes appear to be linked to RA. Hormonal changes during and after pregnancy, while breastfeeding, and even oral contraceptive use may be linked to the development of RA or may relieve or trigger its symptoms.
- Age : RA can affect anyone at any age, but the risk increases with age and usually develops between the ages of 40 and 60.
- Environment : Infection can trigger RA in people who have a genetic link to RA. However, it is important to remember that you cannot catch or spread RA.
- Smoking : Numerous studies have shown that smoking is the most important environmental risk for the development of RA and for a more severe form of the disease.
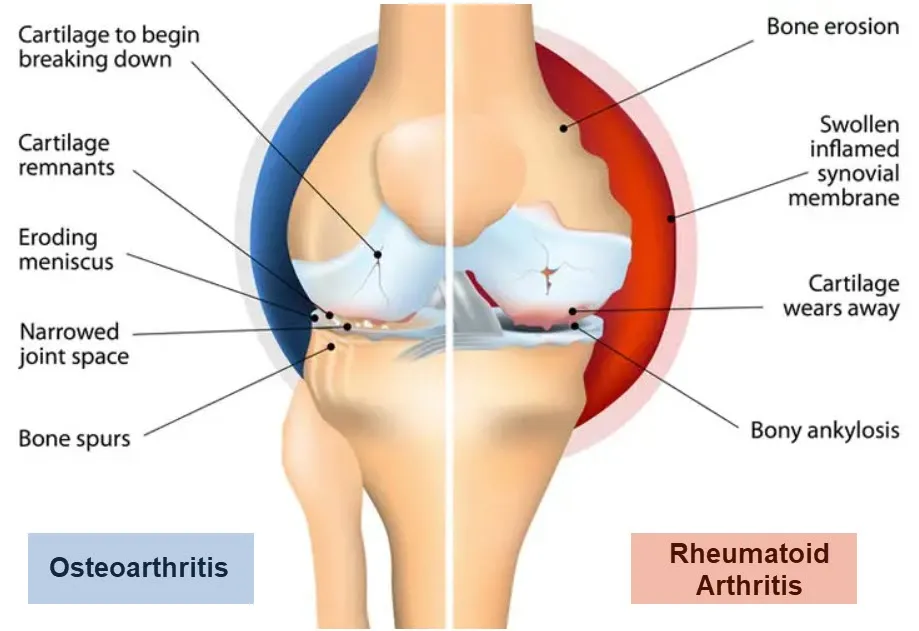
Comparison between Rheumatoid Arthritis and Arthrosis
Rheumatoid Arthritis
- Rheumatoid arthritis is an autoimmune disease.
- Onset – Develops and worsens over several weeks or months.
- Location –Can occur in any joint. Often in the hands, wrists and feet.
- Joint Stiffness – Stiffness that lasts for hours and takes longer to go away.
- Symptoms: pain, stiffness, inflammation, bumps or nodules, fatigue, fever, loss of appetite.
Arthrosis
- Osteoarthritis is a degenerative joint disease.
- Onset – Develops gradually over the years as the articular cartilage wears away.
- Location – Common in the hip, knee, lower back, neck, feet and finger joints.
- Joint stiffness – Mild in the morning, and occurs after a few hours of inactivity during the day.
- Symptoms: joint pain, stiffness, muscle weakness, reduced movement, crunching.
A Day in the Life of Someone Suffering from Rheumatoid Arthritis
Living with rheumatoid arthritis (RA) is a daily challenge that involves managing pain, stiffness, and fatigue. For someone suffering from RA, each day starts with a struggle and requires careful planning and coping strategies.
Morning Routine:
The day typically begins with a battle against morning stiffness, a hallmark symptom of RA. This stiffness can make it difficult to get out of bed and start the day. Waking up early to allow extra time to move slowly and gently stretch the joints is crucial. Warm showers are a common relief, helping to loosen up stiff joints and reduce discomfort. Using assistive devices, such as grab bars and shower chairs, can make this routine safer and more manageable.
Once out of the shower, applying topical pain relief creams and taking prescribed medications are essential steps. These medications, including NSAIDs, DMARDs, and biologics, help manage inflammation and pain. Breakfast often includes anti-inflammatory foods, like fruits, vegetables, and whole grains, as part of a balanced diet aimed at reducing RA symptoms.
Mid-Morning:
By mid-morning, it’s time to engage in light activities to keep the joints moving. Gentle exercises, such as stretching or yoga, are beneficial. These exercises help maintain joint flexibility and strength without putting too much strain on the body. Balancing rest and activity is crucial, as overexertion can exacerbate symptoms.
For those who work, accommodations may be necessary. Ergonomic workstations with adjustable chairs, desks, and keyboards can help reduce joint strain. Regular breaks to stretch and move around are essential to prevent stiffness. Many people with RA also use voice recognition software to minimize typing, which can be painful on swollen joints.
Afternoon:
Afternoons can be challenging as fatigue often sets in. Energy levels fluctuate, making it important to prioritize tasks and rest as needed. Many individuals find that a short nap or relaxation period helps rejuvenate them for the remainder of the day. Managing stress through mindfulness practices or meditation can also help, as stress can worsen RA symptoms.
For lunch, sticking to an anti-inflammatory diet continues. Omega-3 fatty acids found in fish, nuts, and seeds can help reduce inflammation. Hydration is equally important, so drinking plenty of water throughout the day is encouraged.
Evening:
By evening, pain and stiffness may have increased, making it necessary to slow down and focus on self-care. Warm compresses or heating pads applied to sore joints can provide relief. Gentle massage or physical therapy exercises may also be part of the routine to maintain mobility and reduce pain.
Dinner usually follows the same dietary principles, with a focus on lean proteins, vegetables, and whole grains. Avoiding processed foods and sugars is important, as they can contribute to inflammation.
Nighttime Routine:
As bedtime approaches, ensuring a good night’s sleep is a priority. Sleep is often disrupted by pain, so creating a comfortable sleep environment is crucial. This might include using supportive pillows, a heated blanket, and ensuring the bedroom is cool and dark. Taking a warm bath before bed can help relax the muscles and joints.
Medications taken at night, such as pain relievers or sleep aids, can help improve sleep quality. Establishing a regular sleep schedule and practicing good sleep hygiene are essential for managing fatigue and overall health.
Conclusion:
Living with rheumatoid arthritis requires a comprehensive approach to daily life. Each day involves managing pain, stiffness, and fatigue through a combination of medications, diet, exercise, and self-care strategies. While the challenges are significant, with proper management and support, individuals with RA can lead fulfilling lives. Adjusting activities, seeking accommodations, and prioritizing self-care are key to navigating the complexities of this chronic condition.
Differential diagnoses of rheumatoid arthritis
The differential diagnosis of rheumatoid arthritis (RA) involves the exclusion of other diseases that present with similar symptoms. The following conditions may be considered during the differential diagnosis of RA:
- Reactive arthritis: A form of arthritis that occurs in response to an infection in another part of the body, usually the urinary tract or gastrointestinal tract.
- Psoriatic arthritis: A form of inflammatory arthritis associated with psoriasis, a skin disease.
- Systemic lupus erythematosus (SLE): A systemic autoimmune disease that can affect the joints, skin, kidneys, heart, lungs, and other organs.
- Viral arthritis: Certain viruses can cause joint inflammation, usually temporary.
- Arthritis related to ankylosing spondylitis: A form of arthritis associated with inflammation of the spine, often affecting the sacroiliac joints.
- Gout: A form of arthritis caused by the buildup of urate crystals in the joints, often associated with episodes of acute pain.
- Osteoarthritis: Although osteoarthritis is usually related to normal age-related wear and tear on joints, it can sometimes cause mild inflammation.
- Juvenile idiopathic arthritis (JIA): A form of arthritis that affects children and adolescents, characterized by chronic inflammation of the joints.
- Bursitis: An inflammation of the bursa, a small pocket of fluid between the tendons and bones.
- Lyme disease: A tick-borne bacterial infection that can cause inflammatory arthritis.
- Sjögren’s syndrome: An autoimmune disease that primarily affects the salivary and tear glands, but can also cause inflammation of the joints.
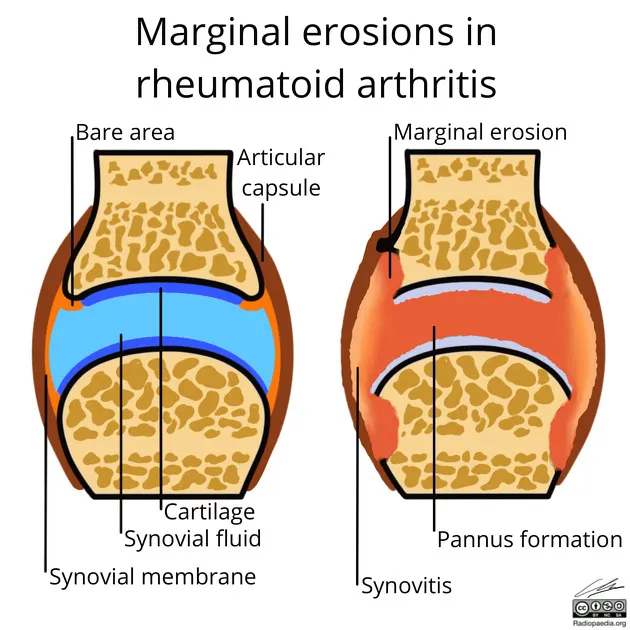
Radiographic Signs of Rheumatoid Arthritis
X-rays remain the primary method for assessing joint damage in RA, although they are not as accurate as cross-sectional imaging such as ultrasound or MRI in detecting signs of inflammatory arthritis. Furthermore, radiographs are often normal in 70% of patients who present to an arthritis clinic at an early stage, despite clinical symptoms suggesting early inflammatory arthritis, and typical radiographic signs are often only visible until in patients whose pathology is well advanced.
Radiological characteristics
- Soft tissue swelling – increased soft tissue shading may be visible, revealing inflammation of the synovium.
- Periarticular osteopenia – inflammation of the joint frequently leads to a reduction in bone mineral density, which is manifested by darker areas adjacent to the joint surfaces on the x-ray.
- Bone erosions – synovial inflammation can invade and damage the cartilaginous and bony surfaces adjacent to the joint, leading to the development of bone erosions which may be visible on x-ray. In RA, these erosions are often called “marginal or juxta-articular bone erosions.”
- Joint space narrowing – cartilage damage due to persistent inflammation can lead to joint space narrowing. In RA, joint space narrowing is generally uniform, reflecting widespread synovial inflammation that affects the entire joint.
- Secondary signs – as the disease progresses, greater bone and cartilage destruction, remodeling, subluxation, dislocation and deformity, for example ulnar deviation at the metacarpophalangeal joints ( MCP).
First radiographic results
- Non -specific periarticular soft tissue swelling with a fusiform configuration
- The fluid found in the joint capsule is overproduced and is composed of:
- Edema
- Synovial hypertrophy (pannus formation)
- Tenosynovitis (and/or)
- Periarticular osteopenia.
Late radiographic findings
- Joint swelling will eventually cause poor joint biomechanics.
- The dislocations will now be subluxations
- Once the subluxation sets in, the joint contact will be more cartilage-cartilage , but rather bone-bone , the contact will now be on the side of the joint
- Indeed, erosion progresses from cartilage-to-cartilage to bone-to-bone.
- This erosion will then be present throughout the joint.
- Joint fusion or ankylosis is a late complication that can occur after complete loss of cartilage.
- Poor joint mechanics will result in secondary osteoarthritis .
- Indeed, this can lead to the formation of:
- Osteophytes
- Subchondral sclerosis
- Subchondral cysts
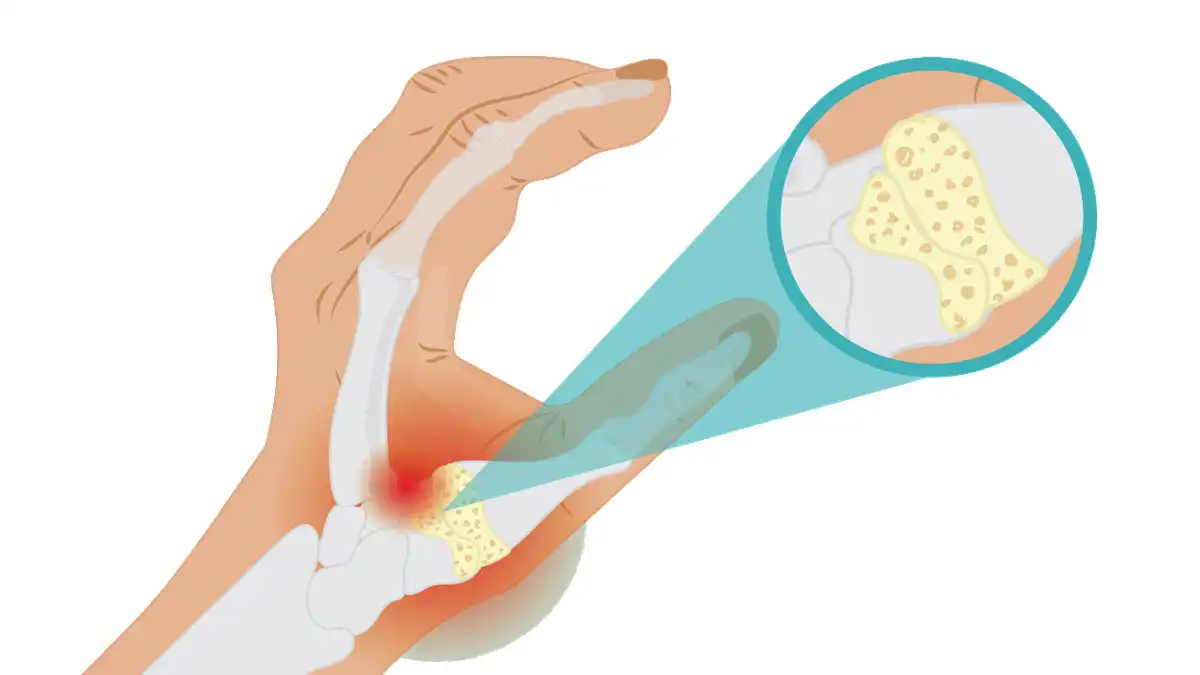
Marginal Erosion
Marginal erosion occurs in the region of the joint that lacks articular contact, specifically where the bone is not covered by cartilage within the joint capsule. The hypertrophic synovium, known as pannus, is responsible for the destruction of bone and cartilage. Erosions are visible on simple radiographs as breaks in the bone surface. Bone erosion results from an increase in osteoclast activity and an inhibition of bone repair mediated by osteoblasts. Erosions typically begin at the intracapsular joint margins, an area of exposed bone between the joint capsule and the start of the cartilage surface. This exposed bone area, called the bare area, lacks thick cartilage and is the first site of erosion in rheumatoid arthritis (RA).

Ankylosis in Rheumatoid Arthritis
As the destruction of cartilage and bone progresses in rheumatoid arthritis, the joint space may be completely obliterated. Ankylosis, characterized by the complete loss of cartilage, represents the terminal phase of this condition. At this advanced stage, joints can fuse together, leading to severe loss of function. Ankylosis is most commonly encountered in specific joints such as the carpus (wrist), tarsus (ankle), metacarpophalangeal joints (knuckles), and proximal interphalangeal joints (middle joints of the fingers). This fusion and consequent immobility mark the final and most debilitating stage of rheumatoid arthritis.
Rheumatoid arthritis of the hand and wrist

- The hands are frequently affected in patients with RA.
- Typical joints involved are
- Articulations métacarpo-phalangiennes (MCP)
- Articulation interphalangienne proximale (IPP)
- Articulations intercarpiennes.
- The first radiographic changes of RA are
- Soft tissue swelling
- Periarticular osteopenia
- Erosions occur early in the disease
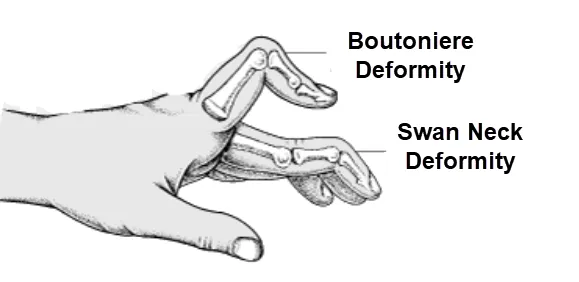
- Joint subluxations are present in more advanced disease and lead to several common deformities:
- Boutonnière deformity (PIP flexion and IPD hyperextension).
- Swan neck deformity (PIP hyperextension and DIPP flexion).
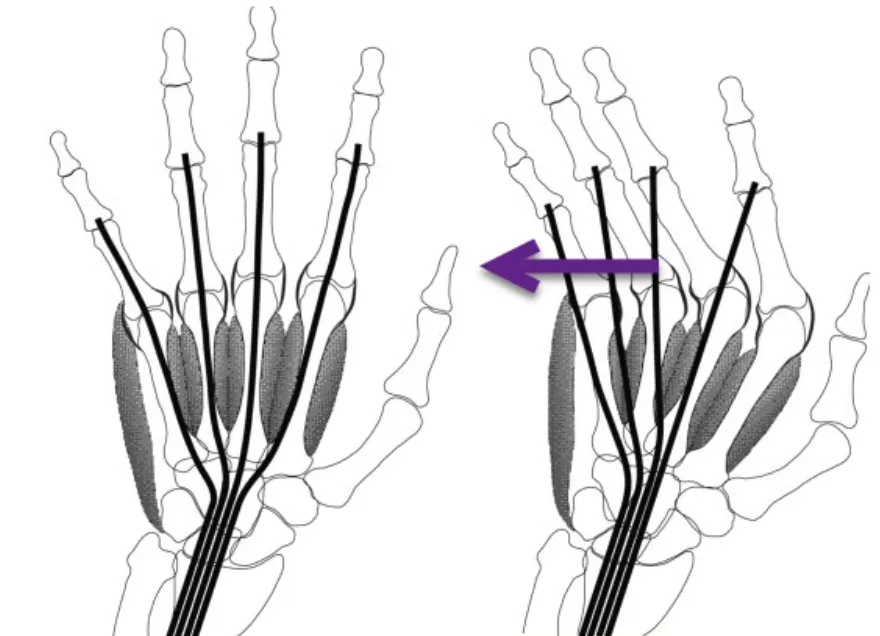
- Ulnar deviation of the fingers at the level of the MCP.

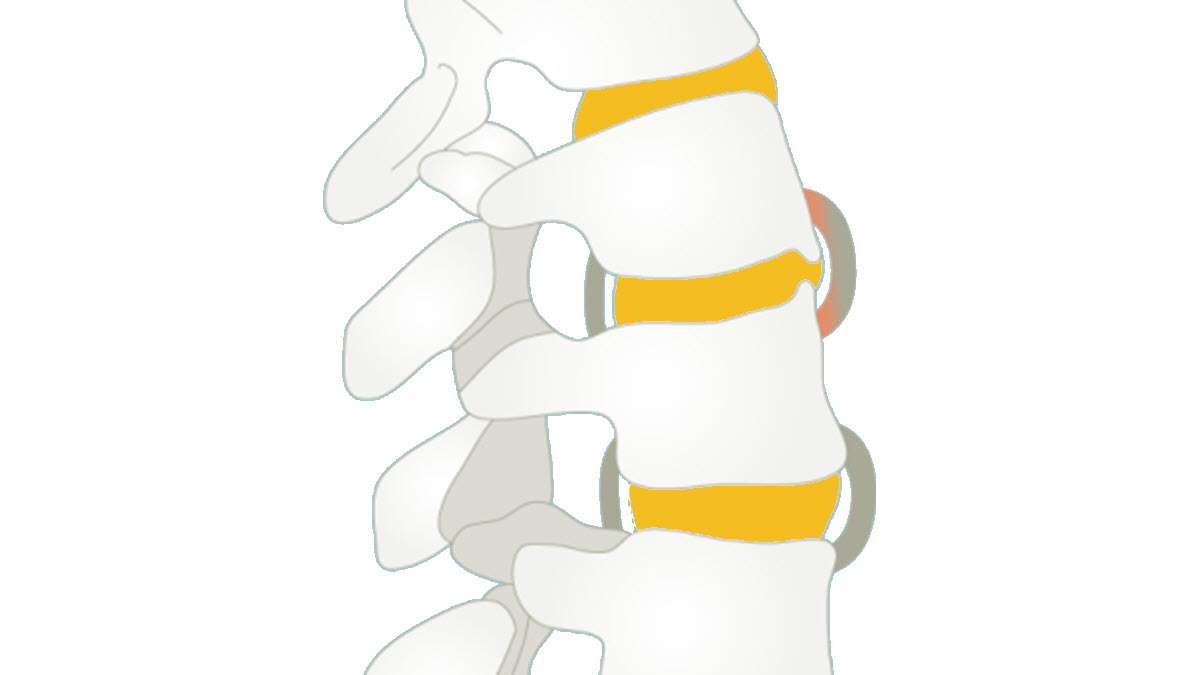
Rheumatoid arthritis of the spine
- The cervical spine is involved in up to 70% of patients.
- Involvement increases with more serious and long-standing illness.
- The thoracic and lumbar spine are almost never involved.
- The general pattern of rheumatoid arthritis in the cervical spine includes:
- Multi-level subluxation
- Osteopenia
- Erosions
- Odontoid
- Facet joints
- Vertebral endplates
- Spinous processes.
- Unlike osteoarthritis, there is no bone production
Before engaging in any form of cervical manipulation, all patients with rheumatoid arthritis should undergo an examination of the cervical spine. Start by taking cervical x-rays, as they help diagnose atlantoaxial instability.
Subluxation Atlantoaxial
This is the most common spinal manifestation of rheumatoid arthritis. Pannus causes erosion of the joint between C1 and C2 and destruction of the transverse ligament and sometimes of the odontoid process. The atlas can then slide forward on C2 and cause compression of the spinal cord. X-rays taken in flexion and extension generally reveal the dynamic nature of the problem and MRI scans provide more detail. There will be an increase in the atlantodental interval and a decrease in the space available for the cord.

The anterior atlanto-dental interval (AIA) is measured from the anterior surface of the odontoid to the posterior surface of the anterior C1 annulus. The IADA is considered abnormal when it is greater than 3 mm in an adult and more than 5 mm in a child.
Symptoms of atlantoaxial rheumatic disease
Atlantoaxial involvement is a condition that affects the junction between the first cervical vertebra (atlas) and the second cervical vertebra (axis), also known as the atlantoaxial joint. This region is crucial because it allows rotational movements of the head. Symptoms of atlantoaxial rheumatic disease can vary depending on the underlying cause, but here are some potential symptoms:
- Neck Pain: Neck pain can be one of the most common symptoms. It can be located at the base of the skull or radiate towards the top of the neck.
- Cervical Stiffness: Stiffness in the cervical region, especially during head rotation movements, may occur due to damage to the atlantoaxial joint.
- Headaches: Headaches, particularly in the back of the head, may be present due to muscle tension and irritation of the structures around the atlantoaxial joint.
- Numbness or tingling: Abnormal sensations in the arms, shoulders, or neck may occur due to nerve compression following atlantoaxial damage.
- Balance problems: Severe impairment can affect balance and coordination due to the impact on the nervous system.
- Difficulty swallowing: In some cases, atlantoaxial damage can cause difficulty swallowing due to the proximity of the cervical structures to the throat.
Conclusion
In conclusion, the active attack on the inflammatory system associated with joint disorders such as rheumatoid arthritis causes devastating changes in the joints and soft tissues. This inflammation leads to swelling of the fusiform tissues and juxta-articular osteoporosis, creating an environment conducive to the breakdown of cartilage and bone. The resulting loss of these essential structures can cause joint misalignment, joint space narrowing, and even joint ankylosis.
Rheumatoid arthritis, as a chronic inflammatory disorder, remains a complex etiological conundrum. It primarily impacts synovial joints, often beginning in small peripheral joints before progressing symmetrically toward proximal joints. Categorizing the disease as early or established is based on the duration of symptoms.
The central aspect of the problem lies in the immune system’s attack on the tissues that cushion the joints, leading to widespread joint deterioration. The process, although poorly understood, leads to joint pain, loss of mobility, and ultimately destruction of the targeted joints.
Despite the uncertainties surrounding the etiology of rheumatoid arthritis, medical research continues to advance in the understanding of this disease. Efforts are being made to uncover specific mechanisms and develop more targeted treatments, with the hope of preventing disease progression and improving patients’ quality of life.
Pending these advances, management of rheumatoid arthritis relies on reducing inflammation, relieving symptoms, and preserving joint function. The multidisciplinary treatment approach, combining specific medications, physiotherapy and psychological support, remains crucial to offer affected individuals the best chance of maintaining an optimal quality of life despite the challenges posed by this debilitating autoimmune disease.
Quiz
Questionnaire 1
- What is special about inflammation in rheumatoid arthritis?
- a) It stimulates the growth of cartilage.
- b) It promotes bone regeneration.
- c) It breaks down cartilage and bone.
- d) It has minimal impact on joint tissues.
- e) It leads to joint ankylosis.
- What are the potential symptoms of atlantoaxial involvement in rheumatoid arthritis?
- a) Neck pain, stiffness, headaches.
- b) Fever, fatigue, weight loss.
- c) Numbness, tingling, balance problems.
- d) Joint pain, swelling, subcutaneous bump.
- e) Morning stiffness, reduction of movements, crunches.
- What is the main target for rheumatoid arthritis?
- a) The long bones of the body.
- b) Cartilaginous joints.
- c) Peripheral muscles.
- d) Ligaments and tendons.
- e) Internal organs.
- What can result from progressive loss of cartilage and bone in rheumatoid arthritis?
- a) Synovial hypertrophy.
- b) Uniform narrowing of the joint space.
- c) The formation of osteophytes.
- d) An increase in joint mobility.
- e) Strengthening of ligamentous structures.
- What is the most common age for the development of rheumatoid arthritis?
- a) Between 20 and 30 years old.
- b) Between 30 and 40 years old.
- c) Between 40 and 50 years old.
- d) Between 50 and 60 years old.
- e) After 60 years.
- What joints are most commonly affected by rheumatoid arthritis?
- a) Hips and knees.
- b) Shoulders and elbows.
- c) The small joints of the hands and feet.
- d) The spine and wrists.
- e) The joints of the toes and fingers.
- What can atlantoaxial instability cause in the cervical spine?
- a) Joint ankylosis.
- b) An atlantoaxial subluxation.
- c) A formation of osteophytes.
- d) A narrowing of the joint space.
- e) Synovial hypertrophy.
- What is the consequence of pannus formation in rheumatoid arthritis?
- a) Strengthening the ligaments.
- b) Ligamentous, cartilaginous and bone destruction.
- c) A decrease in joint mobility.
- d) An increase in bone density.
- e) Improved joint function.
- What are the main radiographic signs of rheumatoid arthritis?
- a) Periarticular osteopenia, bone erosions, narrowing of the joint space.
- b) Soft tissue swelling, wrist fusion, synovial hypertrophy.
- c) Formation of osteophytes, ulnar deviation, subchondral sclerosis.
- d) Marginal erosions, joint subluxations, subchondral cysts.
- e) Damage to internal organs, rheumatoid nodules, fever.
- When is it recommended to take cervical x-rays in patients with rheumatoid arthritis?
- a) Before any drug treatment.
- b) When they feel neck pain.
- c) Before any surgical intervention.
- d) Regularly to detect atlantoaxial instability.
- e) Only in case of serious symptoms.
Answers:
- c
- a
- b
- b
- c
- c
- a
- b
- a
- d
References
- Pujalte GG, Albano-Aluquin SA. Differential Diagnosis of Polyarticular Arthritis. Am Fam Physician. 2015 Jul 01;92(1):35-41. [PubMed]2.
- Jafarzadeh SR, Felson DT. Updated Estimates Suggest a Much Higher Prevalence of Arthritis in United States Adults Than Previous Ones. Arthritis Rheumatol. 2018 Feb;70(2):185-192. [PMC free article] [PubMed]3.
- Murphy LB, Sacks JJ, Helmick CG, Brady TJ, Barbour KE, Hootman JM, Boring MA, Moss S, Guglielmo D, Theis KA. Arthritis Prevalence: Which Case Definition Should Be Used for Surveillance? Comment on the Article by Jafarzadeh and Felson. Arthritis Rheumatol. 2019 Jan;71(1):172-175. [PMC free article] [PubMed]4.
- Murphy L, Helmick CG. The impact of osteoarthritis in the United States: a population-health perspective: A population-based review of the fourth most common cause of hospitalization in U.S. adults. Orthop Nurs. 2012 Mar-Apr;31(2):85-91. [PubMed]5.
- Goldring SR, Goldring MB. Changes in the osteochondral unit during osteoarthritis: structure, function and cartilage-bone crosstalk. Nat Rev Rheumatol. 2016 Nov;12(11):632-644. [PubMed]6.
- Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. 2010 Sep 25;376(9746):1094-108. [PubMed]7.
- Pereira D, Ramos E, Branco J. Osteoarthritis. Minutes Med Port. 2015 Jan-Feb;28(1):99-106. [ PubMed ]8.
- Li R, Hatcher JD. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 29, 2023. Gonococcal Arthritis. [PubMed]9.
- Meng G, Zhu Q, Shao J, Zhang Q, Liu L, Wu H, Xia Y, Bao X, Gu Y, Wang H, Shi H, Sun S, Wang X, Zhou M, Jia Q, Wang G, Song K, Wu Y, Niu K. Comparing the diagnostic ability of inflammatory markers in metabolic syndrome. Clin Chim Acta. 2017 Dec;475:1-6. [PubMed]10.
- Oliviero F, Galozzi P, Ramonda R, de Oliveira FL, Schiavon F, Scanu A, Punzi L. Unusual Findings in Synovial Fluid Analysis: A Review. Ann Clin Lab Sci. 2017 May;47(3):253-259. [ PubMed ]11.
- Ibrahim M, Suzuki A, Yamada K, Takahashi S, Yasuda H, Dohzono S, Koike T, Nakamura H. The relationship between cervical and lumbar spine lesions in rheumatoid arthritis with a focus on endplate erosion. J Spinal Disord Tech. 2015 Apr;28(3):E154-60. [PubMed]12.
- Hassan S. Overview of musculoskeletal ultrasound for the clinical rheumatologist. Clin Exp Rheumatol. 2018 Sep-Oct;36 Suppl 114(5):3-9. [PubMed]13.
- Mitran C, Barbulescu A, Vreju FA, Criveanu C, Rosu A, Ciurea P. Musculoskeletal Ultrasound in Early Rheumatoid Arthritis – Correlations with Disease Activity Score. Curr Health Sci J. 2015 Jul-Sep;41(3):213-218. [PMC free article] [PubMed]