Introduction
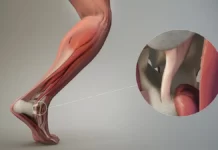
Knee extensor ruptures are complex injuries that affect the stability and function of this crucial joint. The knee extensor system is made up of the quadriceps, patella, patellar tendon and patellar ligament. These structures work in concert to enable knee extension, an essential movement in everyday activities such as walking, running and stair climbing. Ruptures of this device can result from a variety of causes, ranging from acute trauma to repetitive strain.
One of the most common ruptures within the extensor system is the rupture of the patellar tendon. This tendon, connecting the patella to the tibia, allows extension of the knee. Direct trauma, such as a fall on a bent knee or a sudden and intense muscular contraction of the quadriceps, can lead to rupture of this tendon. Symptoms often include an inability to actively extend the knee, swelling, bruising, and significant pain.
Another common rupture is a tear of the quadriceps tendon, which is the tendon of the quadriceps muscle inserting into the kneecap. This type of rupture can occur due to overuse, sudden muscle contraction, or direct trauma to the kneecap. Affected individuals may experience noticeable weakness when extending the knee and feel severe pain.
Patella fractures constitute another category of ruptures of the extensor system of the knee. These fractures can result from a direct force on the kneecap or from excessive strain exerted during flexion or extension of the knee. Typical symptoms include severe pain, swelling, and significant limitation of knee movement.
Treatment of ruptures of the extensor system of the knee depends on the severity of the injury. For partial or less severe tears, non-surgical approaches such as physical therapy may be recommended to strengthen the surrounding muscles and restore knee function. However, in cases of complete or severe ruptures, surgery may be necessary to repair the injured tissue, often followed by a period of intensive rehabilitation.
Prevention of ruptures of the knee extensor system is crucial, particularly in individuals engaged in demanding physical activities. Proper warm-up, use of appropriate protective equipment, and adoption of correct training techniques are important measures to reduce the risk of such injuries.
Definition
Maintaining an upright position depends greatly on the effectiveness of the knee extensor apparatus, a system essential to the functionality of this complex joint. This apparatus consists of the quadriceps and its tendon, the patella and the patellar tendon, which attaches to the anterior tibial tuberosity. The four distinct muscle heads of the quadriceps, namely the vastus medialis, vastus intermedius, vastus lateralis, and rectus femoris, converge distally to form the quadriceps tendon, which attaches to the upper pole of the patella.
The patella, articulated on the femoral trochlea, plays a crucial role in increasing the lever arm of the quadriceps by 30%. This increase in lever arm helps decrease the force needed to extend the knee. The patellar tendon divides, on the one hand, to attach to the lower pole of the patella and, on the other hand, to attach to the anterior tibial tuberosity. These elements align coherently to form an integrated biomechanical unit, essential for active knee extension.
The rupture of any one of these elements, whatever it may be, results in a total inability to actively extend the knee. Although these injuries are rare, their detection is crucial because, according to a study by Siwek and Rao in 1981, 28% of ruptures are not initially diagnosed. Thus, a thorough clinical examination is of paramount importance, because it allows a rapid diagnosis to be established, an essential key to optimal therapeutic care.
The complexity of the knee extensor apparatus highlights the need for a thorough understanding of its components and their interaction to ensure the stability and functionality of this major joint of the body. In the event of an injury, whether it affects the quadriceps, the patella or the patellar tendon, early diagnostic intervention and appropriate treatment are imperative to prevent subsequent complications and restore mobility of the knee.
Causes of Knee Extensor System Ruptures
The causes of knee extensor system ruptures encompass a range of factors, each contributing to the vulnerability of this critical anatomical structure. One primary cause lies in traumatic incidents, such as sports injuries or accidents, where sudden and excessive force is applied to the knee joint, leading to ligamentous or tendon damage. Additionally, chronic overuse or repetitive stress can weaken the knee extensor system over time, making it more susceptible to rupture during routine activities or athletic endeavors. Certain biomechanical abnormalities, including misalignment of the patella (kneecap) or structural deficiencies in the surrounding tissues, can also predispose individuals to knee extensor system injuries. Furthermore, age-related degenerative changes, such as osteoarthritis or tendon degeneration, can weaken the integrity of the extensor mechanism, increasing the likelihood of rupture. Inflammatory conditions, such as tendinitis or bursitis, may exacerbate tissue fragility and predispose individuals to traumatic rupture events. Additionally, systemic factors such as nutritional deficiencies or metabolic disorders can compromise the overall health and resilience of the knee extensor system, potentially contributing to its vulnerability to injury. Moreover, inadequate warm-up or stretching routines before physical activity, coupled with poor conditioning or muscle imbalance, may further elevate the risk of knee extensor system ruptures. Environmental factors, such as uneven terrain or improper footwear, can also play a role in precipitating traumatic events leading to extensor mechanism injuries. Overall, a multifactorial interplay of biomechanical, physiological, and environmental elements underpins the causes of knee extensor system ruptures, necessitating comprehensive assessment and targeted preventive strategies to mitigate the risk of injury and optimize musculoskeletal health.
Add your title here
- Direct trauma: A direct impact on the kneecap, such as a fall on the bent knee or a violent blow, can lead to rupture of the extensor apparatus structures.
- Sudden muscle contraction: A sudden, forceful contraction of the quadriceps muscle can place excessive force on the patellar tendon, potentially leading to a tear.
- Overuse: Repetitive movements or excessive use of the knee, particularly during intensive sporting activities, can contribute to fatigue of the extensor structures, increasing the risk of rupture.
- Indirect trauma: Certain sudden movements, such as excessive twisting of the knee, can place abnormal stresses on the structures of the extensor system, potentially leading to ruptures.
- Anatomical malformations: Anatomical abnormalities, such as irregularities in the shape of the patella or muscular imbalances, can predispose the knee to damage to the extensor system.
- Age: Ruptures of the extensor system of the knee may also be associated with aging, where the quality of connective tissues may decline, increasing vulnerability to injury.
- Improper training techniques: Improper training techniques, such as inappropriate exercises or poor posture during physical activity, can contribute to premature wear and tear of extensor structures.
- Genetic factors: Some individuals may have a genetic predisposition to structural abnormalities or poor tissue strength, increasing the risk of ruptures.
- Arthritis: Forms of arthritis, such as rheumatoid arthritis, can cause inflammation of the knee joints, weakening the extensor structures and increasing the risk of ruptures.
- Poor vascularization: Inadequate blood flow to the knee area can compromise tissue health and increase susceptibility to injury.
- Metabolic diseases: Certain metabolic conditions, such as diabetes, can alter the quality of connective tissues, making extensor structures more vulnerable to rupture.
- Nutritional Deficiency: A lack of essential nutrients, such as vitamins and minerals needed for healthy bones and tendons, can contribute to tissue fragility.
- Joint instability: Problems related to knee joint instability, such as frequent dislocations, can increase stress on the extensor apparatus, increasing the risk of ruptures.
- Poor Posture: Improper posture during walking, running, or other activities can result in uneven distribution of forces across the knee, increasing stress on the extensor apparatus.
- Hormonal Changes: Certain medical conditions or life phases, such as menopause in women, can cause hormonal changes that can affect the health of connective tissues.
- Professional activities: Certain occupations that involve repetitive knee movements or uncomfortable positions can increase the risk of ruptures of the extensor system.
- Clotting disorders: Blood clotting problems can increase the risk of clots, leading to vascular complications in the knee area.
- Congenital anatomical defects: Some individuals may be born with anatomical abnormalities of the knee, such as joint malformations or irregularities in the structure of the tendons, increasing the risk of ruptures.
- Age-Related Degenerative Changes: Aging can lead to degenerative changes in knee tissues, including cartilage, tendons and ligaments, increasing vulnerability to injury.
- Autoimmune conditions: Autoimmune diseases, like lupus, can cause systemic inflammation that can affect joints and tendons, increasing the risk of injury.
- Prolonged use of certain medications: Certain medications, such as corticosteroids, used long-term can weaken connective tissues, making extensor structures more likely to rupture.
- High-risk sporting activities: Participation in high-risk sports, such as football, rugby or downhill skiing, where the knee is subjected to significant forces, can increase the likelihood of injury.
- Repetitive trauma: Frequent exposure to repeated trauma, even of low intensity, can accumulate microtrauma in the structures of the knee, contributing to the risk of ruptures.
- Overall physical condition: Poor general physical condition, including muscle weakness or muscle imbalance, can compromise knee stability and increase the likelihood of injury.
- Obesity: Excess weight can put additional pressure on the knee joints, increasing stress on the extensor system and thus promoting ruptures.
- Hormonal changes associated with pregnancy: Hormonal changes during pregnancy can affect joint stability, potentially increasing the risk of knee injuries.
- Environmental factors: Environmental conditions, such as uneven walking or running surfaces, can contribute to falls and knee injuries.
Symptoms of Knee Extensor System Ruptures
Symptoms of knee extensor system ruptures manifest in various ways, reflecting the complex interplay of anatomical structures involved in knee function. One prominent symptom is acute pain, often localized around the front of the knee or patellar region, particularly upon movement or weight-bearing activities. This pain may be sharp and intense, exacerbating with activities such as climbing stairs, jumping, or squatting. Swelling and inflammation are also common symptoms accompanying knee extensor system ruptures, indicative of the body’s inflammatory response to tissue damage. The affected area may appear visibly swollen, tender to the touch, and exhibit warmth, reflecting the underlying tissue trauma and associated vascular changes.
Functional impairment is a hallmark symptom of knee extensor system ruptures, impacting the individual’s ability to perform activities of daily living and participate in physical exercise or sports. Instability and weakness in the knee joint are frequently reported, with sensations of giving way or buckling, particularly during weight-bearing tasks or sudden movements. Patients may experience difficulty straightening or bending the knee fully, along with limitations in range of motion due to pain and mechanical restrictions imposed by the injured tissues. Moreover, crepitus, or a grinding sensation, may be present during joint movement, indicative of abnormal friction between damaged structures within the knee extensor mechanism.
Alterations in gait and movement patterns are often observed in individuals with knee extensor system ruptures, as they attempt to compensate for pain and instability. This may manifest as a limp or favoring of one leg over the other, as well as changes in posture to offload stress from the injured knee. Furthermore, muscle weakness and atrophy in the quadriceps (front thigh muscles) may develop secondary to disuse and pain inhibition, further exacerbating functional deficits and contributing to ongoing joint instability. In some cases, patients may also experience referred symptoms, such as discomfort or stiffness in surrounding areas of the lower limb, including the hip or ankle, as compensatory mechanisms and altered movement patterns affect the biomechanics of the entire kinetic chain.
Additionally, symptoms of knee extensor system ruptures can have a significant impact on the individual’s psychological well-being and quality of life, leading to frustration, anxiety, and fear of further injury. Sleep disturbances and limitations in daily activities may arise due to persistent pain and functional limitations, further exacerbating the overall burden of the condition on the individual. Overall, the symptoms of knee extensor system ruptures encompass a spectrum of physical, functional, and emotional manifestations, highlighting the importance of comprehensive assessment and management strategies tailored to address the multidimensional impact of this musculoskeletal injury.
- Pain: Sharp or severe pain in the kneecap, patellar tendon, or quadriceps may be felt, particularly during active knee extension.
- Swelling: An increase in knee size due to synovial fluid buildup may occur, causing visible swelling and sometimes a feeling of tightness.
- Hematoma: The formation of a hematoma or bruise around the affected area may be observed, especially in cases of patellar tendon rupture or more serious injuries.
- Limitation of mobility: Difficulty actively extending the knee may occur, and in some cases, joint mobility may be significantly reduced.
- Tenderness to touch: The area around the kneecap, patellar tendon, or quadriceps may be tender to touch, with a feeling of pain or discomfort.
- Muscle weakness: Weakness in the quadriceps may be noticeable, especially when attempting knee extensions.
- Crepitations or noises: Some patients may feel or hear crepitations, grinding, or abnormal noises when they move their knee.
- Inability to bear weight: In severe cases, an inability to bear weight on the affected knee may occur, leading to difficulty walking or standing.
- Visible deformation: In cases of severe rupture, visible deformation of the patella or patellar tendon may be observed.
Pathophysiology of Knee Extensor System Ruptures
The pathophysiology of knee extensor system ruptures involves a cascade of biomechanical and structural changes within the knee joint, leading to compromised integrity and function of the extensor mechanism. One primary mechanism underlying these ruptures is traumatic injury, often occurring during activities that impose excessive or sudden forces on the knee, such as sports-related collisions, falls, or direct blows to the patella. The sudden application of force can exceed the tensile strength of the ligaments, tendons, and other supporting structures, resulting in partial or complete tears within the extensor mechanism.
Chronic overuse or repetitive stress represents another significant pathophysiological mechanism contributing to knee extensor system ruptures. Prolonged and repetitive activities, such as running, jumping, or squatting, can lead to microtrauma and cumulative tissue damage within the extensor mechanism, weakening its structural integrity over time. This chronic wear and tear may predispose individuals to acute ruptures or exacerbate pre-existing degenerative changes within the knee joint, such as patellar tendinopathy or quadriceps tendinosis.
Structural abnormalities and biomechanical imbalances within the knee joint also play a crucial role in the pathophysiology of extensor system ruptures. Malalignment of the patella, such as patellar subluxation or dislocation, can place excessive stress on the surrounding ligaments and tendons, increasing the risk of rupture. Similarly, deficiencies in muscle strength or coordination, particularly in the quadriceps muscles, can alter the distribution of forces across the knee joint, predisposing certain regions of the extensor mechanism to heightened stress and vulnerability to injury.
Degenerative changes associated with aging, such as osteoarthritis or tendon degeneration, further contribute to the pathophysiology of knee extensor system ruptures. These degenerative processes compromise the structural integrity of the ligaments, tendons, and cartilage within the knee joint, rendering them more susceptible to rupture with minimal trauma or stress. Inflammatory conditions, such as tendinitis or bursitis, may also exacerbate tissue fragility and predispose individuals to traumatic rupture events within the extensor mechanism.
Moreover, systemic factors, including nutritional deficiencies, metabolic disorders, and hormonal imbalances, can impact the overall health and resilience of the knee extensor system, influencing its susceptibility to injury and impaired healing processes. The multifactorial nature of knee extensor system ruptures underscores the importance of comprehensive assessment and management strategies aimed at addressing the underlying pathophysiological mechanisms and optimizing musculoskeletal health to prevent recurrence and promote optimal recovery.
- Patellar tendon rupture: This injury occurs when the tendon that connects the kneecap to the shinbone ruptures. Causes may include sudden muscle contractions, direct trauma, or excessive strain during knee flexion or extension. Rupture of the patellar tendon results in loss of continuity of the extensor mechanism, thereby compromising the ability to actively extend the knee.
- Rupture of the quadriceps tendon: This rupture occurs when the tendon formed by the convergence of the muscular heads of the quadriceps ruptures. The causes may be similar to patellar tendon rupture. This injury results in loss of quadriceps integrity, leading to muscle weakness and difficulty performing knee extension.
- Rupture of the patella: Although less common, a rupture of the patella can occur in cases of direct trauma, impact or excessive force. This can lead to joint instability, visible deformation, and significant consequences on knee mobility.
- Anatomical and biomechanical alterations: Ruptures of the extensor system can modify the normal anatomical and biomechanical characteristics of the knee. For example, loss of integrity of the extensor mechanism may compromise stabilization of the patella in the femoral trochlea, thereby increasing the risk of dislocation or subluxation.
- Inflammatory responses and healing: Following a rupture, the body reacts with an inflammatory response aimed at repairing the damaged tissues. However, the healing process can result in the formation of scar tissue, which can influence the functionality and flexibility of the repaired structures.
- Associated Complications: Ruptures of the extensor apparatus may be accompanied by complications such as bone fractures, ligament damage, or other associated injuries. These complications can worsen the severity of the lesion and influence the overall pathophysiology.
Prevention
Prevention of ruptures of the knee extensor system is essential to minimize the risk of serious injuries and associated consequences. Here are some preventative measures that can help reduce the risk of knee extensor ruptures:
- Muscle strengthening: Adopting a regular exercise program focused on muscle strengthening, with particular emphasis on the quadriceps muscles, can improve knee stability and reduce stress on the extensor system.
- Proper warm-up: Before any intense physical activity, it is crucial to do a proper warm-up to prepare the muscles, tendons and ligaments for exercise, thereby reducing the risk of injury.
- Proper Training Techniques: Ensuring you use correct training techniques, especially during sporting activities or lifting weights, can help avoid undue stress on the knee.
- Use of Protective Equipment: For high-risk activities, such as contact sports, it is recommended to use appropriate protective equipment, such as knee pads, to provide additional support to the extensor apparatus.
- Avoid sudden movements: Avoiding sudden movements and rapid changes in direction can reduce stress on knee structures and prevent trauma.
- Maintaining a Healthy Body Weight: Maintaining a body weight within a healthy range can help reduce pressure on the knee joints, thereby decreasing the risk of injury.
- Fall prevention: Taking precautions to prevent falls, especially in older adults, can reduce the risk of knee trauma and extensor system ruptures.
- Flexibility Program: Incorporating flexibility exercises into the workout routine can improve the flexibility of muscles and tendons, thereby reducing strain on the knee.
- Monitoring risk factors: Certain medical conditions, such as osteoporosis, can increase the risk of fractures. Regular monitoring of these risk factors can enable appropriate preventive intervention.
- Medical Consultation: Individuals with a history of knee injuries, underlying medical conditions, or specific concerns should consult a healthcare professional for personalized advice on preventing extensor apparatus ruptures.
Treatment
Treatment of knee extensor ruptures depends on the severity of the injury, the type of rupture, and the specific structures affected. Here is an overview of treatment approaches that may be considered:
- Conservative treatment:
- Immobilization: In some cases of partial or less serious ruptures, immobilization of the knee using a splint or orthosis may be recommended to promote healing.
- Osteopathy: A rehabilitation program supervised by a physical therapist may include strengthening, stretching and proprioception exercises to restore muscle function, stability and mobility.
- Surgical treatment:
- Patellar tendon or quadriceps tendon repair: In cases of complete tears, particularly of the patellar tendon or quadriceps tendon, surgery may be necessary to restore continuity to the injured tissues. This may involve direct repair of the tendons or the use of reconstructive techniques.
- Patella repair: For ruptures of the patella, surgery may be considered to realign and repair the bone fragments. In some severe cases, fixation with screws or other devices may be necessary.
- Grafts and plastics: In some cases, tendon grafts or plastics (using tissue from another region of the body) may be necessary to restore function of the extensor apparatus.
- Pain and inflammation management:
- Medications: Pain relievers and anti-inflammatories may be prescribed to relieve pain and reduce inflammation.
- Orthotics and walking aids:
- Knee pads and splints: Supportive devices such as knee pads may be recommended to provide additional support during the healing phase.
- Medical monitoring :
- Regular consultations: Regular follow-up with the orthopedic surgeon and the rehabilitation team is important to evaluate the progress of healing and adjust the treatment plan if necessary.
References
- Barge-Caballero G, López-Bargiela P, Pombo-Otero J, Pardo-Martínez P. Quadriceps tendon rupture in wild-type transthyretin amyloidosis (ATTRwt). Eur Heart J. 2019 Apr 21;40(16):1307. [ PubMed ]2.
- Wu W, Wang C, Ruan J, Wang H, Huang Y, Zheng W, Chen F. Simultaneous spontaneous bilateral quadriceps tendon rupture with secondary hyperparathyroidism in a patient receiving hemodialysis: A case report. Medicine (Baltimore). 2019 Mar;98(10):e14809. [ PMC free article ] [ PubMed ]3.
- Leciejewski M, Królikowska A, Reichert P. Polyethylene terephthalate tape augmentation as a solution in recurrent quadriceps tendon ruptures. Polim Med. 2018 Jan-Jun;48(1):53-56. [ PubMed ]4.
- Hsu D, Anand P, Mabrouk A, Chang KV. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): May 29, 2023. Biceps Tendon Rupture of the Lower Limb. [ PubMed ]5.
- Colombelli A, Polidoro F, Guerra G, Belluati A. Patellar and quadriceps tendons acute repair with suture anchors. Acta Biomed. 2019 Jan 14;90(1-S):209-213. [ PMC free article ] [ PubMed ]6.
- Nori S. Quadriceps tendon rupture. J Family Med Prim Care. 2018 Jan-Feb;7(1):257-260. [ PMC free article ] [ PubMed ]7.
- Shah MK. Simultaneous bilateral rupture of quadriceps tendons: analysis of risk factors and associations. South Med J. 2002 Aug;95(8):860-6. [ PubMed ]8.
- Shah M, Jooma N. Simultaneous bilateral quadriceps tendon rupture while playing basketball. Br J Sports Med. 2002 Apr;36(2):152-3; discussion 153. [ PMC free article ] [ PubMed ]9.
- SCUDERI C. Ruptures of the quadriceps tendon; study of twenty tendon ruptures. Am J Surg. 1958 Apr;95(4):626-34. [ PubMed ]10.
- Glick R, Epstein DS, Aponso DT. Spontaneous bilateral quadriceps tendon rupture associated with norfloxacin. Intern Med J. 2015 Dec;45(12):1313-5. [ PubMed ]11.
- Yepes H, Tang M, Morris SF, Stanish WD. Relationship between hypovascular zones and patterns of ruptures of the quadriceps tendon. J Bone Joint Surg Am. 2008 Oct;90(10):2135-41. [ PubMed ]12.
- Ciriello V, Gudipati S, Tosounidis T, Soucacos PN, Giannoudis PV. Clinical outcomes after repair of quadriceps tendon rupture: a systematic review. Injury. 2012 Nov;43(11):1931-8. [ PubMed ]13.
- Mosler E, Folkhard W, Knörzer E, Nemetschek-Gansler H, Nemetschek T, Koch MH. Stress-induced molecular rearrangement in tendon collagen. J Mol Biol. 1985 Apr 20;182(4):589-96. [ PubMed ]14.
- Sasaki N, Shukunami N, Matsushima N, Izumi Y. Time-resolved X-ray diffraction from tendon collagen during creep using synchrotron radiation. J Biomech. 1999 Mar;32(3):285-92. [ PubMed ]