Introduction
Trigger finger, also known as stenosing tenosynovitis, is a painful condition affecting the tendons of the fingers, usually most common in the thumb, index, middle, or little finger. This condition is characterized by restricted movement of the fingers, often accompanied by a clicking or popping sound when flexing or extending. The main cause of trigger finger is inflammation of the flexor tendon, which slips through a synovial sheath during finger movement. When this sheath thickens or narrows due to inflammation, the tendon may have difficulty moving smoothly, causing the finger to temporarily become stuck in a bent position.
Risk factors for trigger finger include repetitive activities that strain the finger tendons, such as repeatedly grasping objects or playing musical instruments. People with inflammatory diseases such as rheumatoid arthritis are also more likely to develop this condition. Additionally, trigger finger may be linked to repetitive trauma or microtrauma, increasing strain on the tendons.
Symptoms of trigger finger include a stuck or snapping sensation when flexing or extending the finger, often accompanied by pain at the base of the finger. In some cases, the finger may become stuck in a bent position, requiring manual intervention to straighten it. Symptoms can vary in severity, and some individuals may experience mild stiffness or pain, while others may face significant difficulty in daily activities.
Treatment for trigger finger depends on the severity of the symptoms. Conservative approaches include rest, ice application, stretching exercises, and the use of immobilization devices. As an osteopath, gentle manipulation techniques can be employed to improve joint mobility and promote healing. In cases that are more severe or resistant to conservative treatments, options such as corticosteroid injections or, in some cases, surgery, may be considered.
Management of trigger finger requires a holistic approach, taking into account the patient’s lifestyle habits, professional activities and medical history. Early intervention can help prevent progression of the condition and restore normal finger function, thereby relieving pain and improving the quality of life of those affected by this delicate condition.
Causes of trigger finger
The causes of trigger finger, also known as stenosing tenosynovitis, primarily lie in inflammatory and structural changes in the tendons of the fingers. Inflammation of the flexor tendon, which slides through a synovial sheath during finger movements, forms the basis of this condition. A major cause is irritation and inflammation of this synovial sheath, often resulting from overuse or repetitive stress of the fingers. Work or personal activities that require repeated movements, such as repeated grasping of objects or extensive use of musical instruments, can contribute to the development of trigger finger.
Risk factors also include underlying medical conditions such as rheumatoid arthritis, which can cause widespread inflammation of the joints, including the tendons of the fingers. People with diabetes may also be more predisposed to trigger finger due to changes in connective tissues related to the disease.
Repetitive trauma or microtrauma to the fingers can also be the cause of trigger finger. Direct injuries, dislocations or repetitive movements of the fingers can lead to local inflammation and disrupt the normal function of the tendons, contributing to restricted movement and pain.
Anatomical variations, such as nodules or thickening of the tendons, may also play a role in trigger finger. These structural abnormalities can create additional points of irritation during finger movements, increasing the risk of developing this condition.
Age can also be a contributing factor, as connective tissues tend to lose elasticity over time. Older people may therefore be more prone to degenerative changes in the tendons, increasing the risk of developing trigger finger symptoms.
It is essential to note that certain work or leisure activities can increase the risk of developing trigger finger. People exposed to repetitive movements or excessive stress on the fingers should be aware of these potential risks.
- Thickening of the synovial sheath: The synovial sheath surrounding the tendons can thicken due to inflammation. This can be caused by overuse of the finger, repetitive movements, or trauma.
- Nodule in the tendon: Nodules can form in the tendon, hindering the normal movement of the tendon within the synovial sheath.
- Inflammation of the tendons: Inflammation of the tendons, often related to repetitive activities or excessive movement, can contribute to the development of trigger finger.
- Genetic factors: Some people may be genetically predisposed to developing tendon and synovial sheath problems, increasing the risk of trigger finger.
- Underlying illnesses: Medical conditions such as rheumatoid arthritis, diabetes, or other inflammatory diseases can increase the risk of developing trigger finger.
- Previous injuries: Previous injuries to the fingers, such as sprains or fractures, can contribute to the development of trigger finger.
- Risky occupations or activities: Certain occupations or activities that involve repetitive finger movements or continuous pressure on the hands may increase the risk of stenosing tenosynovitis.
Trigger finger symptoms
The symptoms of trigger finger, also called stenosing tenosynovitis, are often characterized by painful manifestations and limitations of movement in the fingers. One of the warning signs is the sensation of sticking or clicking when flexing or extending a finger, usually accompanied by pain at the base of the finger. This experience may feel like the finger is temporarily stuck in a bent position. The pain associated with trigger finger can vary in intensity, from mild discomfort to sharp pain, depending on the severity of the inflammation and restriction of movement.
People with trigger finger may also experience stiffness in their fingers, especially after a period of rest. In the morning, upon waking, it is not uncommon to experience increased resistance when attempting to move the fingers, which may be accompanied by mild pain. Depending on the severity of the condition, some individuals may experience difficulty fully extending their fingers, leading to a loss of dexterity and functionality in daily activities.
As stenosing tenosynovitis progresses, some individuals may experience fingers getting stuck in a bent position, requiring manual intervention to straighten them. This phenomenon, known as “finger lock,” can cause considerable discomfort and compromise the ability to perform simple gestures. The pain can be localized at the base of the finger, but it can also radiate along the flexor tendon, thus worsening the discomfort.
The severity of symptoms may vary between individuals, with periods of exacerbation and relief. Repetitive activities that tax the finger tendons, such as frequent grasping of objects or using tools, can make symptoms worse. Additionally, pain associated with trigger finger can influence daily habits, limiting the ability to perform simple movements and potentially leading to a decreased quality of life.
- Blockage or resistance during movement: One of the most common symptoms is difficulty bending or extending the finger. Movement may be hampered and may appear choppy, as if the finger is caught in a bent or extended position.
- Pain: Stenosing tenosynovitis can cause pain associated with movement of the finger. The pain may be felt at the base of the finger, near the palm of the hand, or along the affected tendon.
- Clicking or popping sensation: When the finger is moved, there may be a clicking or popping sensation. This is often due to the tendon’s difficult passage through the thickened synovial sheath.
- Swelling: Mild swelling may occur at the base of the finger due to inflammation of the synovial sheath.
- Warmth to the touch: The affected area may feel slightly warm to the touch due to inflammation.
- Nodule Formation: In some cases, a palpable nodule may form in the affected tendon.
- Possible loss of mobility: If the condition is left untreated, loss of mobility in the finger may worsen over time.
Differential diagnoses of trigger finger
- Arthritis: Arthritis, particularly rheumatoid arthritis, can cause inflammation of the joints, which can lead to stiffness and difficulty with movement similar to those seen in trigger finger.
- Tenosynovitis: Tenosynovitis is an inflammation of the synovial sheath that surrounds the tendons. Although similar to trigger finger, tenosynovitis can affect other parts of the body and can result from a variety of causes, including infections.
- Ganglion: A ganglion is a noncancerous mass that usually forms near joints or tendons. It can cause clicking or popping sensations and be confused with a trigger finger.
- Tendon Injuries: Direct injuries to tendons, such as tears or sprains, can cause symptoms similar to trigger finger.
- Carpal tunnel stenosis: Although more common in the wrist, carpal tunnel stenosis can cause symptoms such as pain and difficulty in movement that can be confused with trigger finger.
- Infections: Infections of the soft tissues or joints can also cause inflammation and difficulty with movement.
- Nerve damage: Nerve damage or nerve compression can cause similar symptoms, especially if the nerves around the finger are affected.
- Systemic Diseases: Some systemic diseases, such as lupus, can cause symptoms similar to trigger finger.
Pathophysiology of trigger finger
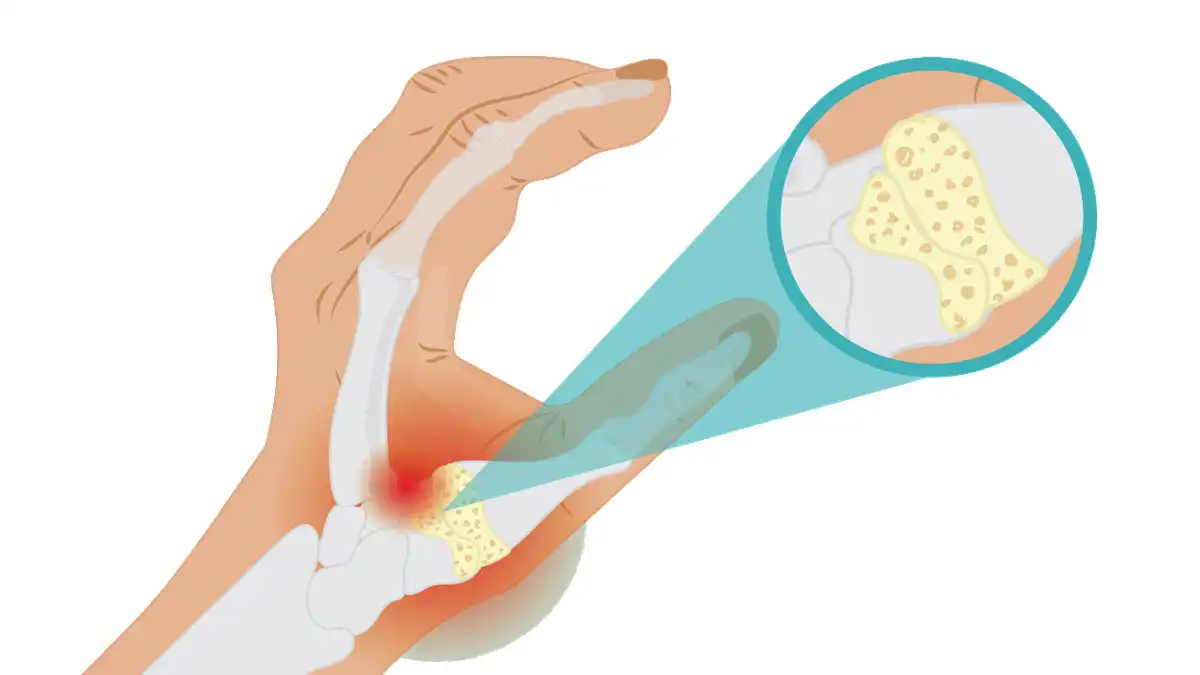
The pathophysiology of trigger finger, also called stenosing tenosynovitis, generally involves changes to the tendons and the synovial sheath that surrounds them. Here is a simplified explanation of the pathophysiology of this condition:
- Tendons and synovial sheath: Tendons are fibrous structures that attach muscles to bones. They allow joint movement by transmitting muscle force to the bones. Tendons slide inside synovial sheaths, structures that provide lubrication to allow smooth movement.
- Inflammation of the synovial sheath: In the case of trigger finger, the pathophysiology often begins with inflammation of the synovial sheath that surrounds the tendon. This inflammation can be caused by overuse of the finger, repetitive movements, previous injuries, or underlying medical conditions such as arthritis.
- Sheath thickening: Chronic inflammation can lead to thickening of the synovial sheath. This creates a smaller space inside the sheath through which the tendon must slide.
- Nodule Formation: In response to inflammation, nodules or thickenings of the tendon itself may form. These nodules can interfere with the normal movement of the tendon within the synovial sheath.
- Restriction of movement: Due to inflammation, thickening of the synovial sheath and nodules, the tendon may have difficulty sliding freely inside the sheath during movement of the finger. This can cause difficulty, a stuck feeling, and possibly a clicking or clicking sound when moving.
Diagnosis and treatment
The diagnosis of trigger finger (stenosing tenosynovitis) is usually based on the clinical examination performed by a healthcare professional. Here are the common steps for diagnosing and treating this condition:
Diagnostic :
- Physical examination: The healthcare professional examines the affected finger, assessing mobility, the presence of nodules, pain, and other symptoms.
- Medical History: Detailed information about the patient’s medical history, including recent activities, previous injuries, and pre-existing medical conditions, is collected.
- Imaging tests: X-rays or ultrasounds may be done to rule out other possible causes of symptoms, such as fractures or joint damage.
Treatment :
- Conservative approaches:
- Osteopathy: Stretching and strengthening exercises may be recommended to improve finger mobility.
- Orthotics: Using immobilization devices, such as splints, can help relieve pressure on the tendon.
- Drugs :
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications can reduce inflammation and relieve pain.
- Corticosteroid injections: Direct injections into the synovial sheath can reduce inflammation.
- Activity management:
- Rest: Avoiding repetitive or excessive finger movements can help relieve symptoms.
- Activity modification: Adapt daily activities to avoid actions that exacerbate symptoms.
- Surgical intervention :
- If conservative treatments do not provide adequate relief, surgery may be considered. The procedure generally involves releasing the synovial sheath to allow smoother movement of the tendon.
- Medical monitoring :
- Regular follow-up with the healthcare professional is important to assess response to treatment, adjust if necessary, and monitor any progression of the condition.
The choice of treatment depends on the severity of symptoms, response to non-invasive interventions, and patient preference. It is essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan, as untreated trigger finger can lead to permanent loss of mobility.
Exercise and stretching
Exercise and stretching can play an important role in managing trigger finger by improving mobility, strengthening muscles, and promoting healing. Here are some exercises and stretches that may be beneficial:
Strengthening exercises:
- Resistance exercise with a rubber band:
- Secure a rubber band around your fingers.
- Slowly spread your fingers against the resistance of the rubber band.
- Repeat several times.
- Passive flexion exercise:
- Use the other hand to gently bend the affected finger.
- Hold the bent position for a few seconds.
- Repeat several times.
- Rolling exercise with a ball:
- Roll a small, firm ball between your palms using moderate pressure.
- Make sure to roll the ball over the entire surface of your palm and fingers.
Stretching:
- Finger stretch:
- Place your hand flat on a surface with fingers extended.
- Use your other hand to apply gentle downward pressure to each finger, stretching the tendons.
- Wrist stretch:
- Extend your arm in front of you with your palm facing down.
- Use the other hand to gently pull the fingers toward you, stretching the wrist muscles and tendons.
- Forearm stretch:
- Extend your arm in front of you with your palm facing up.
- Use the other hand to gently pull the fingers down, stretching the forearm muscles.
- Tabletop hand stretch:
- Place your hand flat on a table with fingers extended.
- Slowly move your body forward to stretch your fingers and wrists.
Additional Tips:
- Heat: Apply a warm compress to the area before exercising to promote blood circulation and flexibility.
- Frequency: Perform these exercises and stretches regularly throughout the day, avoiding exacerbation of symptoms.
Before beginning any exercise program, it is recommended to consult a healthcare professional, including a physiotherapist, to ensure that the exercises are appropriate for your specific situation and are not likely to aggravate the condition.
Questions and answers:
Question 1: What is the sensation described when moving the trigger finger?
a) Tingling
b) Pain
c) Numbness
d) Clicking
Question 2: What is trigger finger also called?
a) Tendinitis
b) Carpal tunnel stenosis
c) Stenosing tenosynovitis
d) Osteoarthritis
Question 3: Which tendons are mainly affected by the pathophysiology of trigger finger?
a) Index finger and middle finger
b) Ring finger and thumb
c) Thumb and little finger
d) Middle finger and little finger
Question 4: What is the role of tendons in joint movement?
a) Attach muscles to bones
b) Maintain finger shape
c) Lubricate joints
d) Stabilize bones
Question 5: What can cause inflammation of the synovial sheath in trigger finger?
a) Sedentary lifestyle
b) Overuse of finger
c) Lack of exercise
d) Too much rest
Question 6: What is the result of synovial sheath thickening in the pathophysiology of trigger finger?
a) Increased mobility
b) Reduction of inflammation
c) Creation of restricted space
d) Nodule formation
Question 7: What is the consequence of the formation of nodules in the tendon?
a) Increased mobility
b) Facilitation of tendon movement
c) Interference with normal tendon movement
d) Decreased pain
Question 8: What are the common symptoms of trigger finger?
a) Numbness and tingling
b) Feeling hot to the touch
c) Difficulty bending or extending the finger
d) Swelling and clicking
Question 9: What is one of the causes of trigger finger related to repetitive activities?
a) Genetic factors
b) Previous injuries
c) Inflammation of the tendons
d) Risky professions or activities
Question 10: What type of exercise is recommended to improve trigger finger mobility?
a) Cardiovascular endurance exercises
b) Strengthening exercises with dumbbells
c) Stretching and strengthening exercises
d) Pressure resistance exercises
- b) Pain
- c) Stenosing tenosynovitis
- b) Ring finger and thumb
- a) Attach muscles to bones
- b) Overuse of the finger
- c) Creation of a restricted space
- c) Interference with normal tendon movement
- c) Difficulty bending or extending the finger
- d) Risky professions or activities
- c) Stretching and strengthening exercises