Introduction
Snapping Hip Syndrome (SHS) is a condition characterized by a snapping or popping sensation felt in the hip joint during certain movements. This snapping sensation may be accompanied by an audible noise and can cause discomfort or pain in the affected area. SHS can be classified into two main types: internal and external snapping hip.
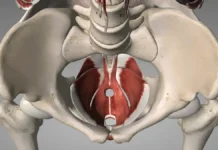
Internal snapping hip occurs when a muscle or tendon slides over a bony prominence within the hip joint, typically the femoral head or the iliopectineal eminence. This can occur when the hip flexor muscles, such as the iliopsoas tendon, pass over these bony structures during activities like walking, running, or cycling. The snapping sensation is usually felt in the front of the hip and may be accompanied by pain or discomfort.
External snapping hip, on the other hand, occurs when a muscle or tendon rubs against the outside of the hip joint. This is often caused by the iliotibial band (IT band) or the gluteus maximus tendon sliding over the greater trochanter of the femur. The snapping sensation is typically felt on the outer side of the hip and may be more pronounced when the hip is extended or rotated.
Osteopathy is a holistic approach to healthcare that focuses on the relationship between the body’s structure and function. Osteopaths believe that the body has the innate ability to heal itself and that optimal health depends on the proper alignment and function of the musculoskeletal system.
In the context of SHS, osteopathy offers a comprehensive approach to assessment, diagnosis, and treatment that addresses both the symptoms of the condition and its underlying causes. Osteopaths use a combination of manual techniques, exercise prescription, and lifestyle advice to restore balance and function to the hip joint and surrounding structures.
Osteopathic treatment for SHS typically begins with a thorough assessment to identify any contributing factors, such as muscle imbalances, joint restrictions, or biomechanical dysfunctions. Osteopaths use palpation techniques to locate areas of tension or restriction in the muscles, tendons, and joints surrounding the hip. They also assess the patient’s posture, gait, and movement patterns to understand how SHS may be affecting their overall musculoskeletal health.
Once the underlying factors contributing to SHS are identified, the osteopath develops a personalized treatment plan tailored to the individual needs of the patient. This plan may include a combination of hands-on manual techniques, such as soft tissue massage, joint mobilization, and stretching exercises, to release tension, improve flexibility, and restore normal movement patterns in the hip joint and surrounding structures.
In addition to manual therapy, osteopathic treatment for SHS often includes therapeutic exercises to strengthen weak muscles, improve flexibility, and correct imbalances in the hip and pelvis. Osteopaths may also provide lifestyle advice to help patients manage SHS symptoms and prevent recurrence, such as recommendations for modifying activities that aggravate symptoms and maintaining proper posture and body mechanics.
Causes of Snapping Hip Syndrome
Overall, osteopathy offers a holistic and individualized approach to the management of Snapping Hip Syndrome, addressing both the symptoms of the condition and its underlying causes to promote optimal musculoskeletal health and function.
Snapping Hip Syndrome (SHS) is a condition that can be caused by a combination of anatomical, biomechanical, and lifestyle factors affecting the hip joint and surrounding tissues. Understanding these underlying causes is essential for effectively diagnosing and treating SHS.
List of Causes:
. Anatomical Abnormalities
- Bony Prominences: Irregularities or prominences within the hip joint, such as a pronounced femoral head or iliopectineal eminence, can lead to the snapping sensation when muscles or tendons pass over them. These abnormalities can be congenital or develop over time due to wear and tear.
- Hip Dysplasia: Structural abnormalities, like hip dysplasia, where the hip socket doesn’t fully cover the femoral head, can increase friction and contribute to the development of SHS.
2. Muscle and Tendon Tightness
- Tight Hip Flexors: The iliopsoas tendon, a key hip flexor, can become tight and cause snapping when it slides over bony structures, especially during hip extension and flexion movements.
- Iliotibial Band (IT Band) Tightness: The IT band, running along the outside of the thigh, can snap over the greater trochanter of the femur, leading to external snapping hip symptoms.
3. Muscle Imbalances
- Weakness in Hip Stabilizers: Imbalances between the hip stabilizing muscles can alter joint mechanics, leading to increased tension and friction within the hip joint.
- Overly Developed Muscles: In some athletes, overly developed or hypertrophied muscles may increase tension around the hip, contributing to snapping sensations.
4. Repetitive Movements and Overuse
- Athletic Activities: Repetitive hip movements common in sports like running, cycling, or dancing can place excessive stress on the hip joint, leading to SHS. Overuse can result in inflammation or tightness of the muscles and tendons around the hip.
- Occupational Factors: Jobs that require repetitive hip movements or prolonged periods of standing can also contribute to the condition.
5. Previous Injuries or Surgeries
- Scar Tissue Formation: Previous hip injuries or surgeries can lead to scar tissue development, which may alter hip biomechanics and cause snapping during movement.
- Altered Mechanics Post-Injury: Changes in the way the hip joint functions after an injury can predispose individuals to SHS due to abnormal movement patterns.
6. Poor Biomechanics
- Gait Abnormalities: Improper walking or running mechanics can increase stress on the hip joint, leading to snapping sensations.
- Postural Issues: Poor posture, such as excessive anterior pelvic tilt or lumbar lordosis, can contribute to the abnormal positioning and movement of the hip, exacerbating SHS symptoms.
7. Structural Conditions
- Arthritis: Hip arthritis can change the shape and function of the joint, leading to increased friction and snapping.
- Synovial Chondromatosis: This condition, characterized by loose bodies within the joint, can cause irregular movement patterns and snapping.
8. Environmental and Lifestyle Factors
- Sedentary Lifestyle: Lack of movement and prolonged periods of inactivity can lead to muscle stiffness and weakness, contributing to the risk of SHS.
- Improper Exercise Techniques: Incorrect form during exercises can place undue stress on the hip joint, leading to snapping sensations.
9. Gender and Age
- Gender: SHS is more commonly observed in women due to anatomical differences in pelvic structure and hormonal influences on ligament laxity.
- Age: Younger individuals, particularly athletes, may experience SHS due to high activity levels, whereas older individuals might develop the condition due to degenerative changes in the hip.
10. Ligament Laxity
- Hyperflexibility: Some individuals naturally have more flexible joints due to ligament laxity, which can lead to increased joint movement and instability. This hypermobility may result in snapping sensations as tendons and ligaments move over bony structures with greater ease.
11. Growth Spurts
- Adolescent Changes: During adolescence, rapid growth can lead to temporary muscle tightness or imbalances as bones grow faster than muscles. This mismatch can cause snapping sensations in active teenagers.
12. Nutritional Deficiencies
- Lack of Essential Nutrients: Deficiencies in key nutrients such as calcium, magnesium, and vitamin D can affect muscle and bone health, potentially leading to imbalances that contribute to SHS.
13. Tendon Inflammation
- Tendinitis: Inflammation of the tendons around the hip, such as iliopsoas or gluteal tendons, can cause swelling and irritation, leading to snapping sensations as these tendons slide over bone.
14. Poor Footwear
- Improper Support: Wearing shoes that do not provide adequate support or cushioning can alter gait mechanics, increasing stress on the hip joint and contributing to snapping hip symptoms.
15. Leg Length Discrepancy
- Unequal Leg Length: A significant difference in leg length can lead to abnormal hip movement patterns, placing uneven stress on the hip joint and increasing the likelihood of snapping sensations.
16. Hip Joint Capsule Tightness
- Restricted Capsule: A tight hip joint capsule can limit the natural movement of the hip, forcing tendons and muscles to compensate by snapping over bony structures.
17. Hormonal Changes
- Hormonal Influence: Hormonal fluctuations, especially in women, can affect ligament laxity and joint stability, potentially contributing to SHS. This is particularly relevant during pregnancy or menstrual cycles when hormonal changes are pronounced.
18. Scar Tissue Adhesions
- Adhesions: Following surgery or injury, scar tissue adhesions can form, restricting normal movement of muscles and tendons, which can lead to snapping sensations during hip motion.
19. Stress Fractures
- Bone Stress: Repeated stress on the hip joint from activities like running or jumping can lead to stress fractures, which may alter hip mechanics and contribute to snapping hip symptoms.
20. Myofascial Restrictions
- Fascia Tightness: The fascia, a connective tissue that surrounds muscles, can become tight or restricted, affecting muscle function and leading to compensatory movements that result in snapping.
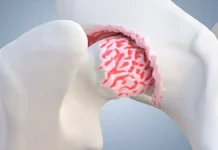
21. Cartilage Damage
- Labral Tears: Damage to the cartilage or labrum within the hip joint can cause friction and instability, leading to snapping sensations as the joint moves.
22. Neuromuscular Control Issues
- Poor Coordination: Neuromuscular control issues, such as delayed muscle activation or poor motor control, can lead to inefficient movement patterns, increasing the risk of SHS.
23. External Trauma
- Injury: Direct trauma to the hip area, such as a fall or blow, can alter the alignment and function of the hip joint, leading to snapping sensations during movement.
24. Compensatory Movements
- Compensation for Injuries: Compensating for injuries or weaknesses elsewhere in the body, such as a sprained ankle or weak core muscles, can place additional stress on the hip joint, leading to SHS.
25. Genetic Predisposition
- Family History: Some individuals may be genetically predisposed to conditions that contribute to SHS, such as certain anatomical traits or joint laxity, which can be inherited.
Symptoms
Snapping Hip Syndrome (SHS) presents with several characteristic symptoms that can vary in severity and frequency among affected individuals. One of the primary symptoms is a snapping or popping sensation felt in the hip joint during certain movements. This sensation may occur with activities such as walking, running, or moving the hip through its full range of motion. The snapping sensation may be audible and palpable, and it is often accompanied by discomfort or pain in the hip region.
In addition to the snapping sensation, individuals with SHS may experience pain or discomfort in the hip joint or surrounding areas. This pain is typically felt as a sharp or dull ache and may be exacerbated by specific movements or activities that trigger the snapping sensation. The pain may be localized to the front, side, or back of the hip joint, depending on the underlying cause of the snapping hip.
Another common symptom of SHS is a feeling of instability or weakness in the hip joint. Individuals may report sensations of the hip “giving way” or feeling unstable during activities that require weight-bearing or movement of the hip joint. This instability may contribute to feelings of discomfort or apprehension when engaging in physical activities, leading to reduced participation in certain sports or recreational activities.
Some individuals with SHS may also experience stiffness or limited range of motion in the hip joint. This stiffness may be most noticeable after periods of inactivity or upon waking in the morning and may improve with gentle movement or stretching exercises. However, excessive stiffness or restricted mobility in the hip joint may exacerbate symptoms of snapping hip and contribute to feelings of discomfort or pain.
In some cases, SHS may be associated with swelling or inflammation in the hip joint or surrounding soft tissues. Swelling may be mild to moderate in severity and may worsen with prolonged or repetitive activity. Individuals may also notice localized tenderness or warmth in the hip joint area, particularly during periods of increased activity or after engaging in strenuous exercise.
Finally, individuals with SHS may experience functional limitations or restrictions in their ability to perform daily activities or participate in sports or recreational activities. The snapping sensation, pain, instability, and stiffness associated with SHS can impact a person’s ability to walk, climb stairs, or engage in activities that require hip mobility and stability. As a result, individuals may experience decreased quality of life and limitations in their overall physical function and participation in daily activities.
Snapping Hip Syndrome (SHS) presents with several characteristic symptoms that can vary in severity and frequency among affected individuals. Here are some common symptoms, along with recommendations for managing them:
List of symptoms and recommendationfor managing them:
Snapping or Popping Sensation
Description: One of the primary symptoms is a snapping or popping sensation felt in the hip joint during certain movements. This sensation may occur with activities such as walking, running, or moving the hip through its full range of motion. The snapping sensation may be audible and palpable.
Recommendations:
- Warm-Up: Engage in a thorough warm-up before any physical activity to increase blood flow and flexibility in the hip area.
- Modify Activities: Avoid or modify activities that trigger the snapping sensation. Gradually reintroduce them as symptoms improve.
- Use Supportive Footwear: Choose shoes with good arch support and cushioning to minimize stress on the hip joint.
2. Pain or Discomfort
Description: Individuals with SHS may experience pain or discomfort in the hip joint or surrounding areas. This pain is typically felt as a sharp or dull ache and may be exacerbated by specific movements or activities that trigger the snapping sensation.
Recommendations:
- Ice Therapy: Apply ice packs to the affected area for 15-20 minutes several times a day to reduce inflammation and pain.
- Pain Relievers: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage pain and reduce inflammation. Consult with a healthcare provider before use.
- Osteopathic Treatment: Consider seeking osteopathic treatment for manual therapy techniques that can help alleviate pain and address underlying causes.
3. Instability or Weakness
Description: A feeling of instability or weakness in the hip joint is common. Individuals may report sensations of the hip “giving way” or feeling unstable during activities that require weight-bearing or movement of the hip joint.
Recommendations:
- Strengthening Exercises: Engage in exercises that strengthen the hip stabilizer muscles, such as hip bridges, clamshells, and leg lifts.
- Balance Training: Incorporate balance exercises, like standing on one leg or using a balance board, to improve hip stability.
- Professional Assessment: Consult an osteopath or physiotherapist for an assessment and personalized exercise plan to address muscle imbalances.
4. Stiffness or Limited Range of Motion
Description: Some individuals with SHS may experience stiffness or limited range of motion in the hip joint. This stiffness may be most noticeable after periods of inactivity or upon waking in the morning.
Recommendations:
- Gentle Stretching: Perform daily stretches targeting the hip flexors, hamstrings, and IT band to improve flexibility and range of motion.
- Foam Rolling: Use a foam roller to gently massage the hip and surrounding muscles to reduce stiffness and improve mobility.
- Yoga or Pilates: Consider yoga or Pilates classes, which focus on flexibility, strength, and alignment, to maintain a full range of motion.
5. Swelling or Inflammation
Description: In some cases, SHS may be associated with swelling or inflammation in the hip joint or surrounding soft tissues. Swelling may be mild to moderate and may worsen with prolonged or repetitive activity.
Recommendations:
- Compression: Use compression wraps or garments to help manage swelling and provide support to the hip joint.
- Elevation: Elevate the affected leg when resting to reduce swelling.
- Anti-Inflammatory Diet: Incorporate anti-inflammatory foods into your diet, such as omega-3-rich fish, nuts, and leafy greens, to help reduce inflammation.
6. Functional Limitations
Description: SHS can lead to functional limitations or restrictions in performing daily activities or participating in sports or recreational activities. The snapping sensation, pain, instability, and stiffness can impact a person’s ability to walk, climb stairs, or engage in activities that require hip mobility and stability.
Recommendations:
- Activity Modification: Adapt daily activities to minimize stress on the hip. Use assistive devices like canes or walking aids if needed.
- Cross-Training: Engage in low-impact cross-training exercises, such as swimming or cycling, to maintain cardiovascular fitness without aggravating symptoms.
- Rehabilitation Program: Work with a healthcare professional to develop a comprehensive rehabilitation program tailored to your needs and goals.
7. Muscle Tightness
Description: Muscle tightness, especially in the hip flexors, glutes, or IT band, can exacerbate the snapping sensation and contribute to discomfort and restricted movement.
Recommendations:
- Regular Stretching: Incorporate regular stretching routines focusing on the hip flexors, gluteal muscles, and IT band to alleviate tightness.
- Foam Rolling: Use a foam roller or massage ball to target tight muscle groups and release tension.
- Hydration: Maintain proper hydration to support muscle elasticity and recovery.
8. Hip Joint Clicking
Description: Some individuals may experience clicking noises in addition to the snapping sensation in the hip joint, which can be unsettling or uncomfortable.
Recommendations:
- Gradual Warm-Up: Perform a gradual warm-up to ensure the hip joint is properly lubricated before engaging in physical activities.
- Alignment Check: Have a professional assess your posture and alignment to identify any contributing factors.
- Osteopathic Manipulation: Consider osteopathic manipulation techniques to correct any joint misalignments or imbalances.
9. Reduced Athletic Performance
Description: Athletes may notice a decline in performance due to discomfort, instability, or pain in the hip joint, impacting their ability to perform optimally.
Recommendations:
- Specific Training Modifications: Work with a coach or trainer to modify training regimens, focusing on hip stability and strength without aggravating symptoms.
- Rest and Recovery: Ensure adequate rest and recovery periods to prevent overuse injuries and support healing.
- Sports-Specific Therapy: Engage in sports-specific physical therapy to address biomechanical issues and enhance performance.
10. Bursitis
Description: Inflammation of the bursa (bursitis) around the hip joint can occur as a secondary condition, causing pain and swelling.
Recommendations:
- Anti-Inflammatory Medication: Use non-steroidal anti-inflammatory drugs (NSAIDs) as prescribed to reduce inflammation and pain.
- Rest: Allow for rest periods to reduce stress on the affected bursa and prevent further irritation.
- Cold Compress: Apply cold compresses to the affected area to alleviate swelling and discomfort.
11. Night Pain
Description: Some individuals may experience increased pain or discomfort in the hip region during the night, potentially disrupting sleep.
Recommendations:
- Sleep Position Adjustment: Use pillows to support the hips and maintain a neutral position while sleeping to reduce strain.
- Relaxation Techniques: Practice relaxation techniques, such as deep breathing or meditation, to help reduce nighttime pain and improve sleep quality.
- Consultation for Pain Management: Consult a healthcare professional for personalized pain management strategies if nighttime pain persists.
12. Radiating Pain
Description: Pain may radiate from the hip to other areas, such as the groin, thigh, or lower back, due to nerve irritation or referred pain.
Recommendations:
- Identify Triggers: Identify and avoid specific movements or activities that trigger radiating pain.
- Physical Therapy: Engage in physical therapy exercises that target and relieve nerve compression or irritation.
- Posture Correction: Work on correcting posture and alignment to reduce pressure on affected nerves.
13. Fatigue and Weakness
Description: Persistent pain and discomfort can lead to fatigue and a general feeling of weakness in the hip and surrounding areas.
Recommendations:
- Gradual Conditioning: Gradually build up strength and endurance through a tailored exercise program to combat fatigue and weakness.
- Balanced Diet: Ensure a balanced diet with adequate nutrients to support energy levels and muscle function.
- Mind-Body Practices: Incorporate mind-body practices, such as yoga or tai chi, to improve energy, balance, and overall well-being.
14. Emotional Distress
Description: Chronic pain and functional limitations associated with SHS can lead to emotional distress, anxiety, or depression.
Recommendations:
- Seek Support: Consider seeking support from a counselor or psychologist to address emotional well-being.
- Stress Reduction Techniques: Practice stress reduction techniques, such as mindfulness or guided imagery, to manage emotional stress.
- Social Engagement: Stay engaged with social activities and support networks to maintain a positive outlook.
15. Hip Joint Stiffness After Prolonged Sitting
Description: Individuals may experience stiffness or discomfort in the hip joint after sitting for extended periods, making it challenging to stand or move comfortably.
Recommendations:
- Frequent Breaks: Take frequent breaks to stand, stretch, and move around if sitting for long periods.
- Ergonomic Seating: Use ergonomic seating that supports proper posture and reduces pressure on the hip joint.
- Hip Mobility Exercises: Incorporate hip mobility exercises into your daily routine to maintain flexibility and prevent stiffness.
16. Decreased Quality of Life
Description: The combined effects of pain, limited mobility, and functional restrictions can lead to a decreased quality of life and impact daily activities.
Recommendations:
- Holistic Approach: Consider a holistic approach to treatment, addressing both physical and emotional aspects of the condition.
- Regular Physical Activity: Engage in regular physical activity, focusing on low-impact exercises that promote overall health and well-being.
- Osteopathic Consultation: Seek an osteopathic consultation for a comprehensive assessment and personalized treatment plan to improve quality of life.
Differential Diagnosis
Differential diagnosis for Snapping Hip Syndrome (SHS) involves distinguishing it from other conditions that may present with similar symptoms. One condition to consider is hip osteoarthritis, which can cause pain, stiffness, and limited range of motion in the hip joint. However, in osteoarthritis, the snapping sensation is typically absent, and symptoms tend to worsen over time rather than with specific movements.
Another condition to consider is hip labral tear, which can cause pain, clicking, or catching sensations in the hip joint. However, labral tears often occur in conjunction with other hip conditions, such as femoroacetabular impingement (FAI), and may present with additional symptoms such as hip locking or instability.
Iliotibial band (IT band) syndrome is another differential diagnosis to consider, especially in cases of external snapping hip. IT band syndrome can cause pain and snapping sensations on the outer side of the hip or knee during activities such as running or cycling. However, IT band syndrome typically presents with pain and tenderness along the lateral aspect of the hip or knee, rather than within the hip joint itself.
Bursitis of the hip, particularly trochanteric bursitis, can also mimic the symptoms of SHS. Trochanteric bursitis typically presents with pain and tenderness over the lateral aspect of the hip, which may be exacerbated by activities such as walking or climbing stairs. However, bursitis typically does not cause snapping sensations within the hip joint itself.
Other less common conditions that may present with snapping hip symptoms include hip dysplasia, synovial chondromatosis, and hip joint infection. These conditions typically present with additional symptoms such as hip instability, joint swelling, or systemic signs of infection, which can help differentiate them from SHS.
Ultimately, the differential diagnosis for SHS involves a comprehensive evaluation of the patient’s symptoms, medical history, physical examination findings, and diagnostic imaging studies such as X-rays, MRI, or ultrasound. By ruling out other potential causes of hip pain and snapping sensations, healthcare providers can accurately diagnose and effectively manage Snapping Hip Syndrome.
Role of Posture
Influence of Posture on Hip Jump
- Pelvic anteversion: Excessive pelvic anteversion, where the pelvis is tilted forward, can increase pressure on the hip, thereby promoting jumping.
- Internal rotation of the hip: A posture that promotes excessive internal rotation of the hip can contribute to compression of the hip structures, increasing the risk of jump.
- Excessive lumbar lordosis: Excessive curvature in the lumbar region can alter spinal alignment and influence hip stability.
- Slouching shoulders and head forward: A slumped posture can lead to muscular imbalances in the pelvic region, which can affect hip function.
Tips for Maintaining Healthy Posture
- Core Engagement: Strengthen the abdominal muscles to support a neutral pelvic position, reducing pressure on the hip.
- Pelvic Stabilization Exercises: Incorporate pelvic stabilization exercises into your workout routine to strengthen the hip stabilizer muscles.
- Hip Flexor Stretches: Practice regular stretches to loosen the hip flexors and prevent excessive anteversion.
- Strengthening Back Muscles: Strengthen the back muscles to maintain a natural lumbar curvature and balance posture.
- Pay Attention to Sitting Position: Avoid sitting for long periods of time without breaks. Use ergonomic chairs and maintain correct sitting posture.
- Warm-up and Stretching Before Exercise: Before any physical activity, perform specific warm-ups to prepare the hip and practice appropriate stretching.
- Daily Posture Consciousness: Be aware of your posture throughout the day. Adjust your position regularly to avoid sagging or excessive strain.
- Professional Consultation: Consult a health professional, such as an osteopath, for an assessment of your posture and personalized advice.
Prevention of hip jolt
List:
Hip stretches:
- Hip Flexion: Assume a forward lunge posture with one knee bent forward. Tilt the pelvis slightly forward to stretch the hip of the back leg.
- External Rotation: Sitting, cross the ankle over the opposite knee and apply light downward pressure on the knee to stretch the external rotation of the hip.
2. Strengthening the stabilizer muscles:
- Hip Bridges: Lie on your back, bend your knees and lift your hips, contracting your buttocks muscles.
- Lateral Leg Raises: Lie on your side and lift your top leg up, engaging your lateral hip muscles.
3. Joint mobility exercises:
- Hip Circles: Standing, draw circles with your knee forward and to the side, making sure to maintain a comfortable range of motion.
- Seated Hip Rotations: Sitting on the floor, bend your knees and do hip rotations in both directions.
4. Ankle Stability Training:
- Balance on one leg: While standing, raise one leg and maintain balance for a few seconds. Repeat on the other side.
- Line walking: Walk on an imaginary line keeping your feet aligned to build ankle stability.
5. Correct movement technique:
- Running or walking technique workshop: Consult a healthcare professional or fitness coach to correct your movement technique, emphasizing a balanced stride.
6. Adequate warming:
- Pre-exercise hip activation: Incorporate hip muscle activation exercises into your warm-up routine to prepare the area for physical activity.
7. Improved fascia flexibility:
- Self-massage with a foam roller: Use a foam roller to gently massage the hip muscles and fascia to improve flexibility.
8. Proprioception exercises:
- Stabilization on a Bosu Ball: Perform stabilization exercises on a Bosu ball to improve proprioception and hip stability.
Muscle Strengthening Exercises for the Hip
Strengthening the hip muscles can be beneficial in alleviating the symptoms of hip jerk. Here is a list of targeted exercises that aim to strengthen the muscles in this region:
List of Muscle Strengthening Exercises for the Hip
**1. Squats
- Stand with your feet shoulder-width apart.
- Go down by bending your knees as if you were sitting, keeping your back straight.
- Return to the starting position, engaging the muscles of your buttocks and hips.
2. Forward lunges
- Step forward with one leg, bending both knees until both are bent 90 degrees.
- Return to the starting position and repeat on the other side.
3. Hip Bridges
- Lie on your back with your knees bent and your feet flat on the floor.
- Slowly lift your hips upward, contracting your buttocks muscles.
- Hold the position at the top for a few seconds, then lower back down.
4. Lateral Leg Raises
- Lie on your side with your top leg slightly forward.
- Lift the top leg up, keeping the leg straight, then lower back down.
5. Hip abductions
- Lie on your side with your legs stacked.
- Lift the top leg up, then lower back down.
6. External hip rotations
- In a seated position, cross one ankle over the opposite knee.
- Apply gentle downward pressure on the knee to stretch and strengthen the hip muscles.
7. Hip flexions in quadruped position
- On all fours, lift one bent leg toward the ceiling, keeping the knee bent at 90 degrees.
- Lower the leg and repeat with the other leg.
8. Step-ups
- Use a sturdy bench or step.
- Go up and down, alternating legs, to strengthen your hip muscles.
9. Side walk with elastic band
- Place an elastic band around the ankles.
- Walk sideways while maintaining constant tension on the band.
10. Plank with hip abduction
- In a plank position, lift one leg out to the side without rotating your trunk.
- Alternate legs.
Preventive or therapeutic muscle stretching
- Stretching the ilitibial band

2. Hip flexor stretch


3. Piriformis Stretch

4. Hamstring Stretch

5. Bridge
Conclusion
In conclusion, Snapping Hip Syndrome (SHS) presents a unique challenge in musculoskeletal medicine, but osteopathic treatment offers a comprehensive approach to address its underlying causes and symptoms effectively. Osteopathy, with its focus on restoring balance and function to the musculoskeletal system, plays a pivotal role in the management of SHS.
Osteopathic treatment for SHS begins with a thorough assessment to identify contributing factors such as muscle imbalances, joint restrictions, or biomechanical dysfunctions. Osteopaths utilize hands-on manual techniques, including soft tissue manipulation and joint mobilization, to alleviate tension, improve mobility, and restore normal movement patterns in the hip joint and surrounding structures.
Additionally, osteopaths prescribe therapeutic exercises tailored to strengthen weak muscles, improve flexibility, and correct imbalances in the hip and pelvis. These exercises aim to provide better stability and support to the hip joint, reducing the risk of snapping sensations and associated symptoms.
Furthermore, osteopathic treatment for SHS includes lifestyle modifications and patient education to help individuals manage symptoms and prevent recurrence. Osteopaths offer guidance on activity modification, posture correction, and self-care techniques to empower patients to take an active role in their recovery.
Overall, osteopathic treatment for SHS emphasizes a holistic approach that addresses both the physical and functional aspects of the condition. By restoring balance and function to the musculoskeletal system, osteopathy offers patients with SHS the opportunity to achieve long-term relief from symptoms, improve mobility, and enhance their overall quality of life.
References
- Hyland S, Graefe SB, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 8, 2023. Anatomy, Bony Pelvis and Lower Limb, Iliotibial Band (Tract) [ PubMed ]2.
- May O. Arthroscopic techniques for treating ilio-psoas tendinopathy after hip arthroplasty. Orthop Traumatol Surg Res. 2019 Feb;105(1S):S177-S185. [ PubMed ]3.
- Nolton EC, Ambegaonkar JP. Recognizing and Managing Snapping Hip Syndrome in Dancers. Med Problem Perform Art. 2018 Dec;33(4):286-291. [ PubMed ]4.
- Snapping Hip Syndrome. Orthop Nurs. 2018 Nov/Dec;37(6):361-362. [ PubMed ]5.
- Badowski E. Snapping Hip Syndrome. Orthop Nurs. 2018 Nov/Dec;37(6):357-360. [ PubMed ]6.
- Flato R, Passanante GJ, Skalski MR, Patel DB, White EA, Matcuk GR. The iliotibial tract: imaging, anatomy, injuries, and other pathology. Skeletal Radiol. 2017 May;46(5):605-622. [ PubMed ]7.
- Macke C, Krettek C, Brand S. [Tendinopathies of the hip: Treatment recommendations according to evidence-based medicine]. Unfallchirurg. 2017 Mar;120(3):192-198. [ PubMed ]8.
- Chang CY, Kreher J, Torriani M. Dynamic sonography of snapping hip due to gluteus maximus subluxation over greater trochanter. Skeletal Radiol. 2016 Mar;45(3):409-12. [ PubMed ]9.
- Potalivo G, Bugiantella W. Snapping hip syndrome: systematic review of surgical treatment. Hip Int. 2017 Mar 31;27(2):111-121. [ PubMed ]10.
- Ilizaliturri VM, Camacho-Galindo J. Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon. Sports Med Arthrosc Rev. 2010 Jun;18(2):120-7. [ PubMed ]11.
- Przybył M, Walenczak K, Lebiedziński R, Domżalski M. Analysis of Arthroscopic Therapy for hip Pathologies. Ortop Traumatol Rehabil. 2017 May 10;19(3):249-261. [ PubMed ]