Carpal tunnel syndrome (CTS) is a condition resulting from compression of the median nerve at the wrist, through an anatomical structure called the carpal tunnel.
Understanding Carpal Tunnel Syndrome: A Narrow Tunnel, a Nerve in Trouble
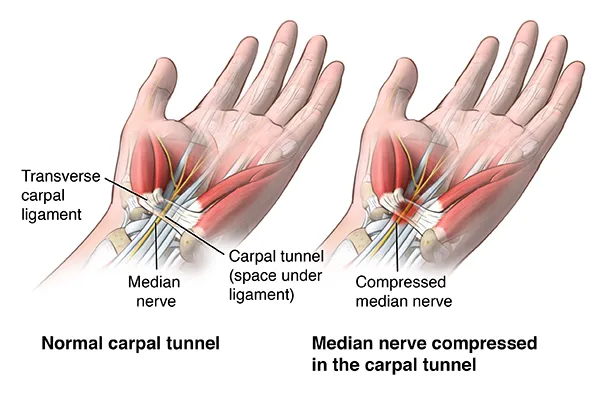
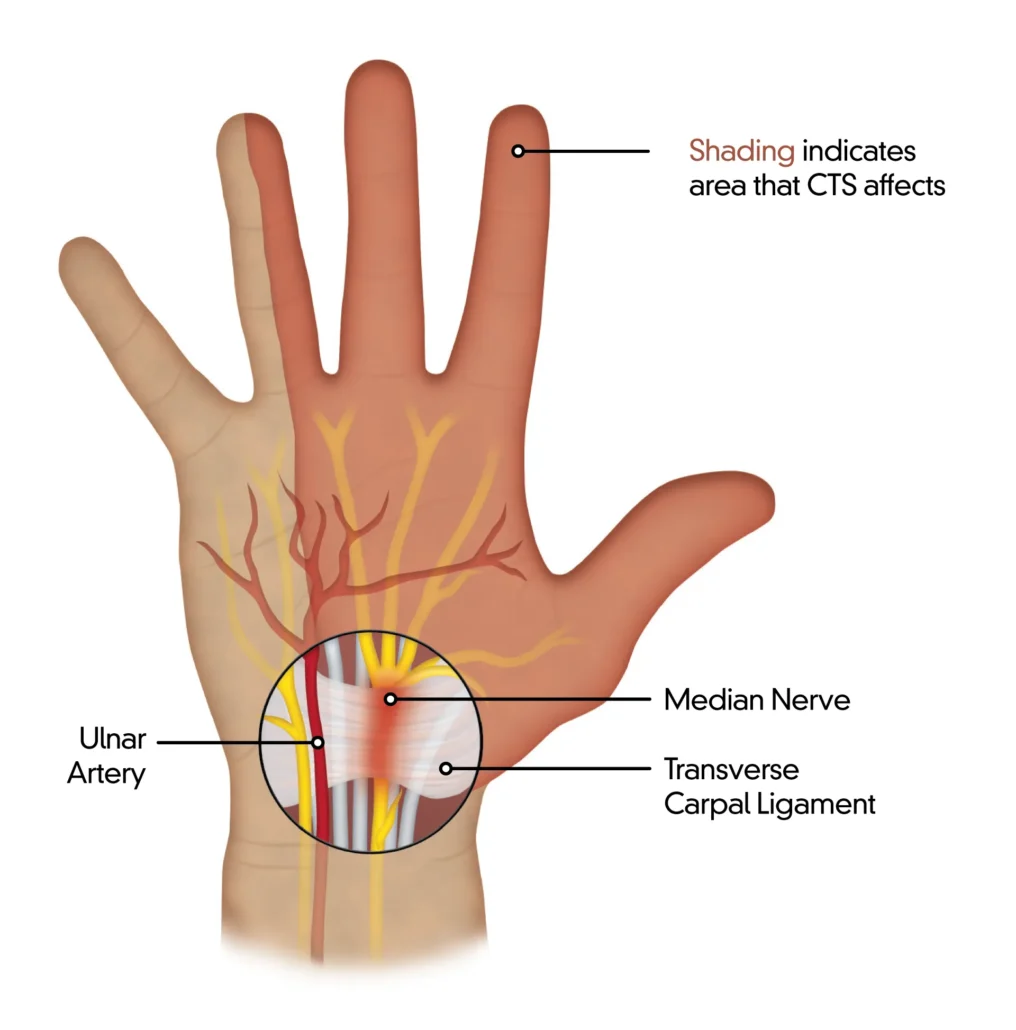
The narrow, rigid pathway formed by the wrist bones and the transverse carpal ligament houses a structure crucial to hand function: the median nerve. This nerve exerts essential control over sensation and muscle function in parts of the hand, including the thumb, index finger, middle finger, and part of the ring finger. This narrow channel, known as the carpal tunnel, is the site where a common problem, carpal tunnel syndrome (CTS), can develop.
CTS, seen in approximately one percent of the population, is often associated with excessively repetitive wrist flexion and extension movements. These repeated gestures can lead to unpleasant sensations such as numbness and tingling along the distribution of the median nerve, thus affecting the three and a half fingers on the lateral side of the hand. This condition is of particular concern due to its impact on the quality of life of affected individuals.
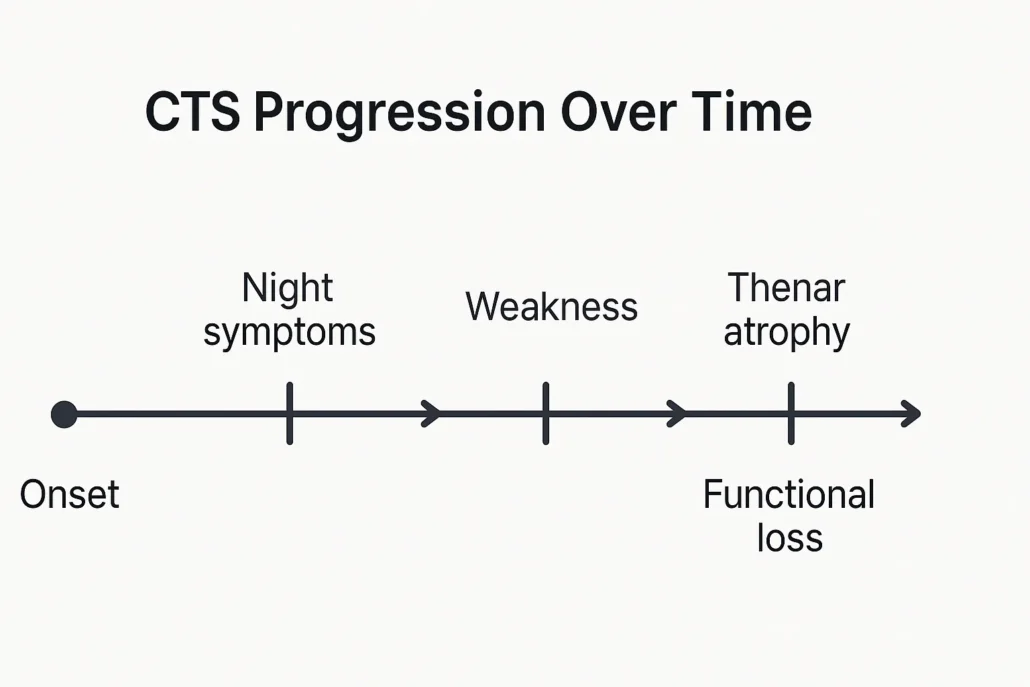
A distinctive aspect of CTS is the presence of nocturnal symptoms, causing painful awakening in those affected. Pain and discomfort can be so severe during the night that it disrupts sleep, adding an additional burden to patients’ daily lives. If this condition persists, atrophy of the thenar muscles may develop, leading to weakness and clumsiness of the thumb and fingers. This progressive deterioration can significantly impair a person’s ability to perform simple tasks of daily living, from grasping objects to performing precise movements.
Carpal tunnel compression represents the most common nerve compression syndrome, with an estimated incidence of approximately 99 cases per 100,000 people. This condition predominates in women, affecting between 65 and 75% of the affected population. It usually manifests in middle age, although cases can also occur in younger individuals, especially those exposed to repetitive movements as part of their work or daily activities.
Management of CTS may vary depending on the severity of symptoms and response to conservative treatments. For mild to moderate cases, wearing splints may be recommended to relieve pressure on the median nerve. Modifications to daily activities to avoid excessive repetitive movements may also be suggested. However, in more severe cases or if there is no relief with conservative treatments, surgery may be considered. Surgical carpal tunnel release is a common and effective procedure to relieve pressure on the median nerve.
In conclusion, CTS, although common, should not be neglected due to its implications on the quality of life of those affected. Understanding symptoms, risk factors, and treatment options is essential for appropriate management of this debilitating condition. Continued research in this area aims to improve prevention and treatment strategies, providing hope for those living with CTS.
What Causes Carpal Tunnel Syndrome? Repetition, Inflammation, and Other Risk Factors
Carpal tunnel syndrome (CTS) represents a prevalent and often debilitating condition characterized by compression of the median nerve within the carpal tunnel of the wrist. This compression results in a range of symptoms, including pain, numbness, tingling, and weakness in the hand and fingers. Understanding the multifaceted causes of CTS is crucial for both prevention and effective management of the condition.
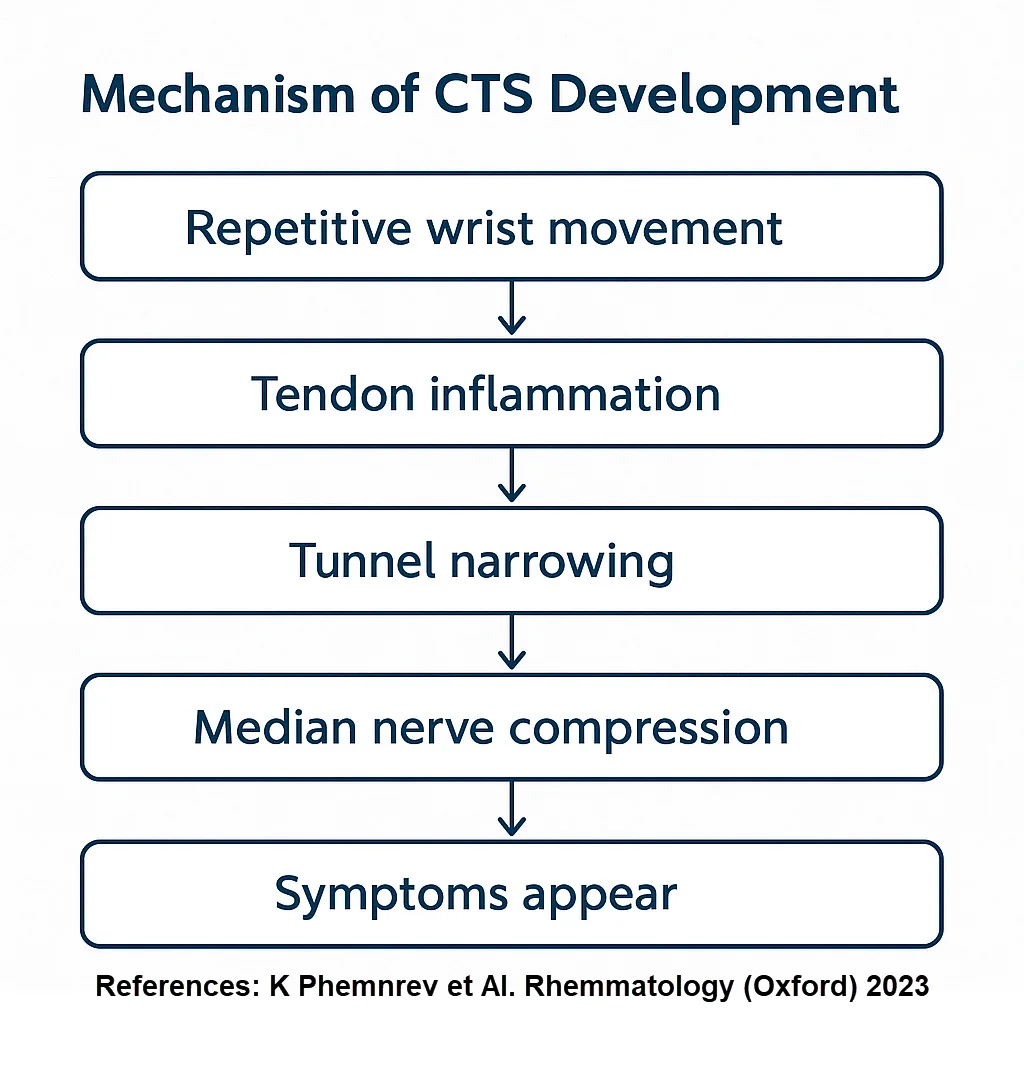
Repetitive hand and wrist movements are widely recognized as significant contributors to the development of CTS. Occupations and activities that involve frequent and forceful use of the hands and wrists, such as typing, using vibrating tools, or performing assembly line work, can lead to repetitive strain injuries. Over time, this repetitive stress can cause inflammation and swelling of the tissues within the carpal tunnel, resulting in compression of the median nerve and the onset of CTS symptoms.
In addition to repetitive movements, acute trauma or injuries to the wrist can also predispose individuals to CTS. Fractures, sprains, or other traumatic injuries can lead to swelling and inflammation of the surrounding tissues, including those within the carpal tunnel. This increased pressure on the median nerve can exacerbate symptoms or trigger the development of CTS in susceptible individuals.
Anatomical factors play a significant role in the pathogenesis of CTS. The carpal tunnel is a narrow passageway in the wrist, through which the median nerve and several tendons pass. Any narrowing or constriction of this tunnel can increase the likelihood of nerve compression. Some individuals may have naturally smaller carpal tunnels, while others may have anatomical variations in the structure of the wrist bones that predispose them to CTS. Conditions such as arthritis or joint dislocations can further contribute to the narrowing of the carpal tunnel, exacerbating nerve compression and CTS symptoms.
Hormonal changes, particularly during pregnancy or menopause, can also impact the risk of developing CTS. Pregnancy-related hormonal fluctuations can lead to fluid retention and swelling in the body, including the tissues within the carpal tunnel. This increased pressure on the median nerve can contribute to the development or worsening of CTS symptoms in pregnant individuals. Similarly, hormonal changes associated with menopause can affect tissue elasticity and fluid balance, potentially increasing the risk of CTS in postmenopausal women.
Several medical conditions are associated with an increased risk of developing CTS. Diabetes, obesity, thyroid disorders, and autoimmune diseases such as rheumatoid arthritis are among the conditions that can affect nerve function and increase susceptibility to nerve compression. Individuals with these underlying medical conditions may be more prone to developing CTS or experiencing more severe symptoms.
Occupational factors also play a significant role in the development of CTS. Jobs that require repetitive hand and wrist movements, prolonged periods of wrist flexion or extension, or exposure to vibrating tools or equipment are considered high-risk for CTS. Workers in industries such as manufacturing, assembly line work, data entry, and construction are particularly susceptible to developing CTS due to the repetitive nature of their tasks.
Lastly, genetic predisposition may contribute to an individual’s risk of developing CTS. While the precise genetic factors involved are not fully understood, some individuals may inherit anatomical characteristics or genetic traits that increase their susceptibility to nerve compression and CTS. Family history of CTS or other nerve-related conditions may also influence an individual’s risk.
Here are some common causes of carpal tunnel syndrome:
- Wrist Anatomy: Some individuals may have wrist anatomy that predisposes them to carpal tunnel narrowing, increasing the risk of median nerve compression.
- Inflammation: Inflammation of the tendons surrounding the median nerve can cause the space in the carpal tunnel to narrow, thereby compressing the nerve.
- Trauma or Injury: Wrist fractures or traumatic injuries can lead to tissue swelling and compression of the median nerve.
- Repetitive Activities: Repetitive wrist movements or activities that involve frequent flexion or extension of the wrist may contribute to the development of carpal tunnel syndrome.
- Medical Conditions:
- Arthritis: Some forms of arthritis, such as rheumatoid arthritis, can cause inflammation of the tissues around the median nerve.
- Diabetes: People with diabetes have an increased risk of developing nerve disorders, including carpal tunnel syndrome.
- Hypothyroidism: Poorly controlled hypothyroidism may be associated with an increased risk of carpal tunnel syndrome.
- Pregnancy: Pregnant women, especially during the third trimester, may develop carpal tunnel symptoms due to fluid retention and hormonal changes.
- Obesity: Excess weight can increase pressure on nerves, including the median nerve.
Inside the Tunnel: How Median Nerve Compression Triggers Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is a medical condition that results from compression of the median nerve at the wrist. The pathophysiology of CTS can be described in several stages:
- Anatomy of the carpal tunnel: The carpal tunnel is a narrow structure located at the wrist, formed by the carpal bones and the transverse carpal ligament. Inside this canal pass several finger flexor tendons and the median nerve.
- Compression of the median nerve: The median nerve is responsible for the innervation of certain parts of the hand, notably the first three fingers and the radial half of the fourth finger. When there is compression of the median nerve, usually due to increased pressure within the carpal tunnel, symptoms of CTS may manifest.
- Causes of compression:
- Inflammation: Inflammation of the flexor tendons can lead to thickening of the structures within the carpal tunnel, thereby compressing the median nerve.
- Trauma: Wrist injuries, such as fractures or sprains, can cause tissue swelling, leading to compression of the nerve.
- Medical Conditions: Certain medical conditions such as rheumatoid arthritis, diabetes, or hypothyroidism can contribute to the development of CTS.
- Reduced space in the carpal tunnel: Increased pressure inside the carpal tunnel reduces the space available for the median nerve. This can lead to decreased blood flow and direct compression of the nerve.
- Symptoms of CTS:
- Numbness and tingling in the fingers.
- Muscle weakness in the hand, especially difficulty grasping objects.
- Pain radiating from the wrist to the arm.
- Disease progression: If compression persists, CTS symptoms may worsen over time. In some severe, untreated cases, this can lead to muscle atrophy and loss of hand function.
- Diagnosis and treatment: The diagnosis of CTS is usually based on clinical symptoms, electrophysiological tests (such as electromyography), and imaging studies. Treatment may include conservative measures such as splints, anti-inflammatory medications, osteopathy sessions, or in some cases, surgery to release pressure in the carpal tunnel.
Recognizing the Symptoms of Carpal Tunnel Syndrome: Numbness, Pain, and Weakness
- Pain: Pain is often felt in the palm of the hand, fingers, especially the thumb, index finger, middle finger and part of the ring finger. The pain may radiate to the forearm.
- Numbness and Tingling: People with carpal tunnel syndrome may experience numbness, tingling, or “tingling” sensations in the affected fingers. These sensations may be intermittent or constant.
- Weakness: Weakness in the hand may develop, leading to difficulty grasping objects, performing fine manual tasks, or maintaining a firm grip.
- Feeling of Swelling: Some people feel a feeling of swelling, even if no swelling is visible.
- Sensation of Warmth: Sensations of warmth may be felt in the affected hand or fingers.
- Worse at Night: Symptoms of carpal tunnel syndrome tend to get worse at night. Some people may be awakened by pain or numbness.
- Electric Shock Sensation: In some cases, people may feel a sensation of electric shock that radiates down the arm.
- Difficulty Using the Hand: Hand function may be impaired, which can make it difficult to perform everyday tasks, such as writing, typing, or grasping objects.
The role of work-related factors in the development of carpal tunnel syndrome remains a matter of controversy in the workers’ compensation context. The literature generally demonstrates that the use of vibrating tools and tasks involving repetitive flexion and extension motions, particularly when combined with high grip strength, are associated with an increased risk of symptomatic carpal tunnel syndrome.
Recognizing the Symptoms of Carpal Tunnel Syndrome: Numbness, Pain, and Weakness
Carpal Tunnel Syndrome (CTS) is a condition that affects the hand and arm, causing numbness, tingling, and pain. For those suffering from CTS, daily life can be a series of challenges and adaptations. Here is a glimpse into a typical day in the life of someone with this condition.
Morning Routine
The day often starts with discomfort. Many individuals with CTS experience increased symptoms during the night due to wrist positioning. As a result, mornings can be particularly tough. The initial struggle is to shake off the numbness and tingling in the hands and fingers. Simple tasks such as turning off the alarm clock or brushing teeth can be painful and frustrating. Using an electric toothbrush with a wider handle might help alleviate some of the discomfort.
Work Challenges
For those who work in jobs that require repetitive hand movements, such as typing or using tools, the workday can be especially grueling. Ergonomic adjustments become essential. A keyboard with a wrist rest, a vertical mouse, and frequent breaks to stretch and rest the hands are necessary adaptations. However, despite these modifications, the persistent discomfort can lead to reduced productivity and increased fatigue.
Daily Activities
Tasks that most people take for granted, like opening jars, gripping utensils, or even holding a phone, can be challenging. Cooking, for example, requires numerous hand movements that can exacerbate pain. Simple solutions, such as jar openers or specially designed kitchen tools, can make a significant difference. For someone with CTS, pacing themselves and taking frequent breaks is crucial to manage pain and prevent further strain.
Physical Therapy and Treatment
Many people with CTS incorporate physical therapy exercises into their daily routine. These exercises help strengthen the muscles in the hand and wrist, improve flexibility, and reduce symptoms. Additionally, some might wear a wrist splint, especially at night, to keep the wrist in a neutral position and minimize pressure on the median nerve.
For some, medication is part of the daily regimen. Over-the-counter pain relievers like ibuprofen or prescribed medications can help manage pain and inflammation. In more severe cases, corticosteroid injections or even surgery might be necessary. However, these treatments come with their own set of challenges and recovery periods.
Social and Emotional Impact
Living with chronic pain and physical limitations can take a toll on mental health. The frustration of being unable to perform everyday tasks, coupled with persistent pain, can lead to feelings of helplessness and depression. Social activities, such as going out with friends or engaging in hobbies, might become less enjoyable due to the constant discomfort. It’s essential for individuals with CTS to seek support from friends, family, or support groups, and to consider speaking with a mental health professional if they feel overwhelmed.
Evening Wind-Down
As the day winds down, the symptoms of CTS might intensify due to the cumulative strain from daily activities. Evening routines often include applying ice packs to reduce inflammation, using topical analgesics, and performing gentle stretches. A warm bath can also help relax the muscles and alleviate some of the discomfort.
Finally, as bedtime approaches, individuals with CTS must take care to position their wrists comfortably to prevent worsening symptoms overnight. Wearing a wrist splint to bed is a common practice to ensure the wrist remains in a neutral position, reducing pressure on the median nerve.
Pregnancy and Carpal Tunnel Syndrome: Hormones, Swelling, and Wrist Pain
Pregnancy is a time of profound physiological transformation, affecting nearly every system in the body. Among the lesser-known but surprisingly common challenges faced by expectant mothers is carpal tunnel syndrome (CTS)—a condition that causes pain, tingling, numbness, and weakness in the hand and wrist. CTS is particularly prevalent during the second and third trimesters, when fluid retention and hormonal changes are most pronounced.
Why Does Pregnancy Trigger CTS?
The median nerve, which controls sensation in the thumb, index, middle, and half of the ring finger, runs through the narrow carpal tunnel in the wrist. Any swelling or compression in this tight space can place pressure on the nerve and lead to the classic symptoms of CTS.
Several factors converge during pregnancy to make this more likely:
1. Fluid Retention
During pregnancy, the body naturally retains more water to support the growing fetus, increase blood volume, and prepare for delivery. Unfortunately, this retention doesn’t always distribute evenly. Soft tissues, including those around the wrists, may swell, especially at night. This swelling can significantly increase pressure in the carpal tunnel, compressing the median nerve.
2. Hormonal Changes
Pregnancy is associated with major shifts in hormone levels, including increased relaxin and estrogen. These hormones help loosen ligaments and soften connective tissues in preparation for childbirth. However, this laxity can also affect the structure of the wrist, potentially reducing the available space in the carpal tunnel and predisposing the area to nerve entrapment.
3. Anatomical Predisposition
Some women may naturally have a narrower carpal tunnel, making them more susceptible to compression when additional swelling occurs. If a woman has experienced wrist pain or CTS symptoms prior to pregnancy—perhaps related to repetitive activities or certain health conditions—she may be at greater risk of symptom recurrence or worsening during pregnancy.
Common Symptoms in Pregnant Women
Pregnancy-related CTS tends to present with:
- Numbness and tingling, especially in the thumb, index, and middle fingers
- Burning pain or weakness in the hand
- Nighttime symptoms that can disturb sleep
- A sense of swelling or tightness in the fingers, even when no swelling is visible
Symptoms can affect one or both hands and may range from mild to severe.
What Can Be Done?
The good news is that in most cases, pregnancy-related CTS is temporary. Symptoms often improve or resolve entirely after delivery, as hormone levels and fluid balance return to baseline.
In the meantime, several strategies can help manage discomfort:
- Wearing a wrist splint, especially at night, to keep the wrist in a neutral position
- Elevating the hands to reduce swelling
- Avoiding repetitive wrist movements or prolonged gripping
- Gentle stretching exercises and, in some cases, osteopathic support
If symptoms are severe or persist after delivery, a healthcare professional may recommend further evaluation or treatment options.
Menopause and Carpal Tunnel Syndrome: Hormonal Shifts and Nerve Sensitivity
Menopause marks a significant transition in a woman’s life, characterized by the natural decline in reproductive hormones, especially estrogen. While not a direct cause of carpal tunnel syndrome (CTS), menopause is increasingly being recognized as a contributing factor in the onset or exacerbation of its symptoms. This relationship is believed to stem from complex interactions between hormonal fluctuations, connective tissue changes, and nervous system sensitivity.
During the perimenopausal and postmenopausal phases, estrogen levels decrease substantially. Estrogen plays a crucial role in maintaining the elasticity and hydration of connective tissues. As its levels decline, tendons and ligaments may become less supple and more prone to thickening or inflammation. Within the carpal tunnel—a confined space bordered by bones and ligaments—such changes can lead to increased pressure on the median nerve, particularly if there is already a predisposition due to repetitive wrist activity or genetic anatomical variations.
Another factor that may link menopause to carpal tunnel symptoms is fluid retention. Although more common during pregnancy, fluid retention can also occur during menopause due to altered hormone balances, particularly fluctuations in aldosterone and estrogen. When this fluid accumulates in the extremities, it can increase pressure within the carpal tunnel, especially at night, contributing to the classic symptoms of CTS: tingling, numbness, and hand discomfort.
Additionally, menopause is often associated with systemic musculoskeletal changes. Loss of bone density, joint stiffness, and increased prevalence of conditions such as osteoarthritis can alter hand and wrist mechanics. These biomechanical changes may further compromise the carpal tunnel’s structure and increase the likelihood of nerve compression.
Sleep disturbances, commonly reported by menopausal women, may also exacerbate CTS. Sleeping with bent wrists, a common position during the night, can elevate intra-carpal pressure and aggravate symptoms. This nocturnal worsening—marked by numbness or a burning sensation in the fingers—can be particularly distressing and affect quality of life.
It is also important to consider the role of central sensitization during menopause. Hormonal changes can impact the nervous system’s sensitivity to pain, potentially lowering the threshold for discomfort and amplifying the perception of nerve irritation. As a result, symptoms of mild or moderate CTS may be felt more acutely in postmenopausal individuals.
Despite these associations, not all menopausal women will develop carpal tunnel syndrome, and other factors such as occupational demands, comorbidities (e.g., diabetes, thyroid dysfunction), and body weight also play essential roles. However, it is important for healthcare practitioners to recognize this link, particularly in women who present with new-onset hand symptoms during or after the menopausal transition.
If you are postmenopausal and experiencing symptoms such as numbness, tingling, hand weakness, or waking up with discomfort in your fingers, it may be worthwhile to consult a healthcare provider. Early evaluation and conservative interventions—such as wrist splints, ergonomic modifications, or osteopathic support—can help manage symptoms effectively and prevent progression.
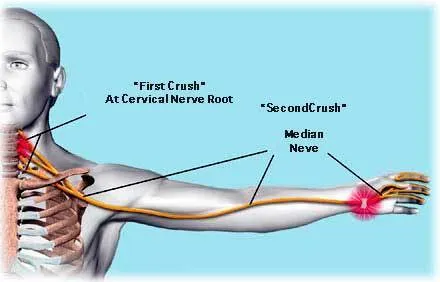
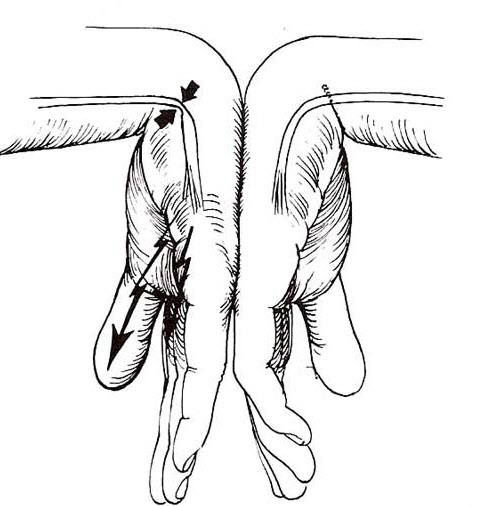
Double Crush Syndrome: When Nerves Are Compressed in More Than One Place
The term Double Crush Syndrome (DCS) was first introduced in 1973 by researchers Upton and McComas. Their hypothesis proposed that a nerve subjected to compression at one point along its pathway becomes more vulnerable to additional compressions elsewhere. In other words, a proximal nerve lesion — such as one in the cervical spine or brachial plexus — may sensitize the distal portion of the same nerve, making it more susceptible to compression at locations like the carpal tunnel. This concept offered a new explanation for persistent or recurrent symptoms, particularly in cases where standard treatments like carpal tunnel release surgery did not yield complete relief.
This theory has been particularly relevant for understanding cases of carpal tunnel syndrome (CTS) that do not fully resolve after decompression surgery. In such scenarios, the presence of a more proximal nerve irritation — for example, a cervical disc herniation, foraminal stenosis, or scalene muscle entrapment — could be contributing to the overall clinical picture. The interaction between multiple compressive sites along the same nerve pathway may result in more severe symptoms than would be expected from any single site of entrapment alone.
“Double Crush Syndrome reminds us that wrist pain may not start at the wrist. Treating nerve compression effectively means considering the whole pathway — from the neck to the hand.”
Clinically, DCS may manifest as a blend of upper limb symptoms: patients can report tingling, numbness, or pain in the hand, wrist, forearm, upper arm, shoulder, or even neck. These symptoms may overlap with classic carpal tunnel syndrome but often extend beyond the median nerve distribution, complicating the diagnosis. For example, a patient with both cervical radiculopathy and CTS might describe pain radiating from the neck to the hand, accompanied by weakness, paresthesia, or clumsiness during fine motor tasks.
One of the most common proximal contributors to double crush phenomena is cervical radiculopathy, particularly involving the C6-C7 nerve roots. These nerve roots contribute to the median nerve, which passes through the carpal tunnel. Any compromise at the cervical level — including degenerative disc disease or osteophyte formation — can reduce axoplasmic flow within the nerve, decreasing its ability to tolerate additional stress downstream. As a result, even a mild entrapment at the carpal tunnel may become symptomatic when combined with cervical irritation.
The concept of double crush syndrome remains somewhat controversial in medical literature. While many clinicians recognize the logic of a multi-level nerve vulnerability, the empirical evidence remains limited and sometimes contradictory. Some studies have failed to find a strong statistical correlation between cervical and distal nerve entrapments, while others have supported the idea of additive effects from multiple compressive sites. It is therefore essential to approach DCS not as a definitive diagnosis, but as a clinical consideration that requires careful assessment.
For osteopathic practitioners and other manual therapists, the double crush concept reinforces the importance of a global and integrative approach. It suggests that local wrist symptoms should not be treated in isolation. A thorough neurological examination, including assessment of the cervical spine, thoracic outlet, brachial plexus, and upper extremity, is critical. Palpation, mobility testing, and neurodynamic assessments can help identify the multiple points of dysfunction along the nerve’s trajectory.
Treatment of double crush syndrome should be individualized and multifaceted. Addressing the distal site (e.g., through splinting or local manual therapy) may help reduce symptoms, but full resolution often requires treating the proximal source as well. This may involve cervical spine mobilizations, postural correction, myofascial release techniques along the scalene or pectoralis minor muscles, and exercises to restore neurodynamic mobility. In some cases, collaboration with neurologists or orthopedic specialists may be necessary to confirm diagnosis and guide advanced interventions.
How Wrist Position Affects Carpal Tunnel Pressure and Nerve Compression
“The Impact of Wrist Positions on Carpal Tunnel Pressure
The pressure within the carpal tunnel varies significantly depending on wrist positioning. Comparative figures highlight stark differences between healthy individuals and those with carpal tunnel syndrome.
At rest, with the wrist in a neutral position:
- Normal: 2.5 mm Hg
- Carpal tunnel syndrome: 32 mm Hg
During 90-degree wrist extension and flexion:
- Normal (average): Approximately 31 mm Hg
- Carpal tunnel syndrome (flexion): 94 mm Hg
- Carpal tunnel syndrome (extension): 101 mm Hg
These measurements underscore a marked elevation in carpal tunnel pressure among individuals with carpal tunnel syndrome, particularly during wrist movement. This heightened pressure significantly contributes to symptoms such as numbness, tingling, and pain associated with the condition.”
Who’s at Risk? Key Factors That Contribute to Carpal Tunnel Syndrome
Here are some of the risk factors associated with carpal tunnel syndrome:
- Repetitive Work or Frequent Hand Strain: People whose jobs involve repetitive hand or wrist movements, such as grasping or heavy tool use, may be at greater risk of developing carpal tunnel syndrome.
- Wrist Position: Prolonged use of the wrist in a flexed or extended position, as may occur when using a computer keyboard or tool, may increase risk.
- Anatomical Factors: Some individuals may have an anatomy that predisposes to a more restricted space in the carpal tunnel, thereby increasing the risk of median nerve compression.
- Gender: Women have a slightly higher risk of developing carpal tunnel syndrome compared to men. This may be related to anatomical and hormonal differences.
- Age: Carpal tunnel syndrome is more common in older people, although it can occur at any age.
- Pregnancy: Hormonal changes during pregnancy and fluid retention can increase the risk of median nerve compression.
- Obesity: Excess weight can increase pressure on nerves, including the median nerve.
- Medical Conditions:
- Rheumatoid Arthritis: People with rheumatoid arthritis have an increased risk due to joint inflammation.
- Diabetes: People with diabetes have a higher risk of developing nerve problems, including carpal tunnel syndrome.
- Wrist Trauma: Wrist injuries, such as fractures or sprains, can increase the risk.
- Use of Oral Contraceptives: Some studies have suggested that long-term use of oral contraceptives may be associated with increased risk.
Carpal Tunnel or Cervical Radiculopathy? How to Tell the Difference
Carpal tunnel syndrome (CTS) and cervical radiculopathy are conditions that can cause similar symptoms in the arms and hands but originate from different anatomical locations and mechanisms.
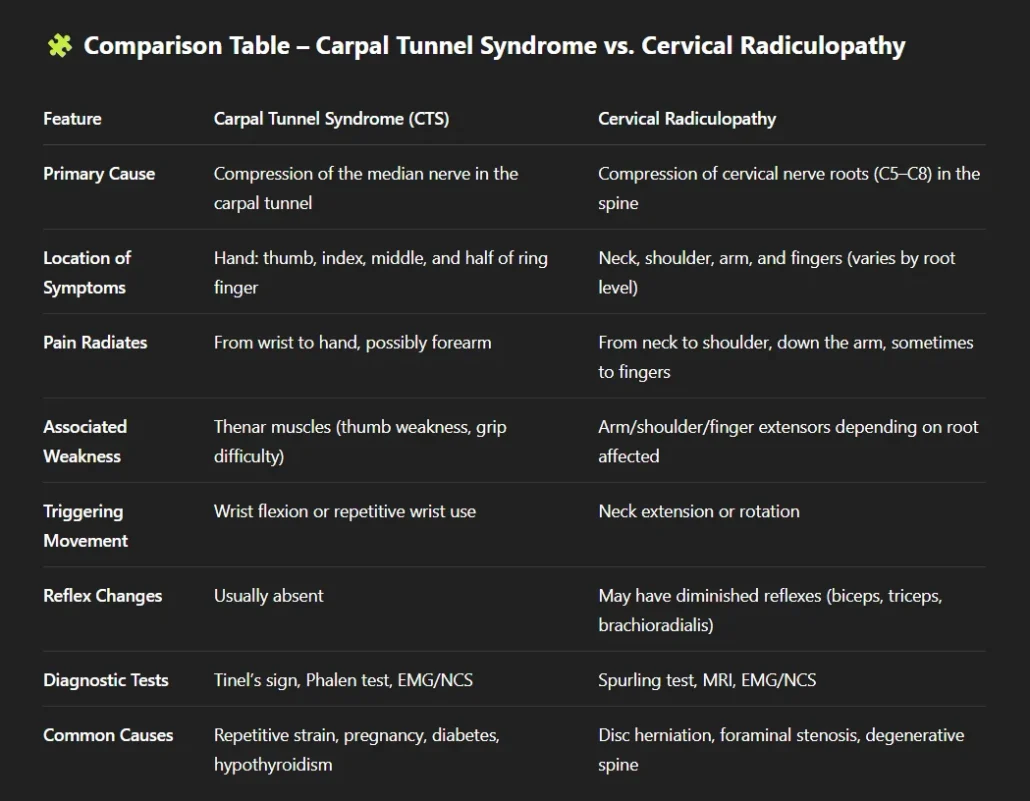
Carpal Tunnel Syndrome
CTS occurs due to compression of the median nerve as it passes through the carpal tunnel in the wrist. Symptoms include:
- Numbness, tingling, and pain in the thumb, index, middle fingers, and half of the ring finger.
- Weakness and difficulty with fine motor tasks.
- Symptoms worsen with wrist movements.
Risk factors include repetitive hand use, wrist injuries, and certain medical conditions. Diagnosis involves clinical evaluation and tests like nerve conduction studies. Treatment ranges from splinting and corticosteroid injections to surgery in severe cases.
Cervical Radiculopathy
This condition results from compression or irritation of nerve roots in the neck, often due to herniated discs or degenerative changes. Symptoms include:
- Neck pain radiating to the shoulder or arm.
- Numbness, tingling, weakness, and loss of reflexes in specific patterns.
- Symptoms may worsen with neck movements or certain positions.
Risk factors include age-related spine changes and neck injuries. Diagnosis involves physical examination, imaging, and sometimes EMG tests. Treatment includes rest, physical therapy, medications, and possibly surgery.
Differences:
CTS primarily affects the hand and is aggravated by wrist movements, while cervical radiculopathy originates in the neck and may involve neck pain and specific arm and hand symptoms related to nerve root patterns.
Clinical Tests for CTS: Tinel’s Sign, Phalen’s Test, and Beyond
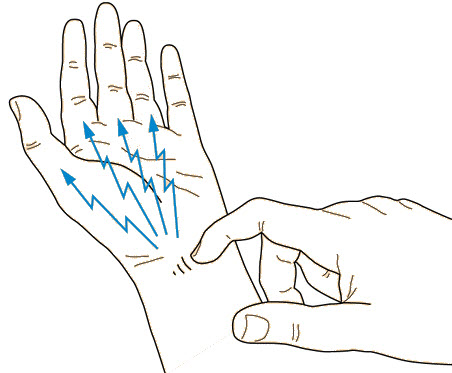
Tinel sign
The Tinel sign at the wrist is often used to assess the presence of nerve disorders, particularly in the context of carpal tunnel syndrome. Here is how the Tinel wrist test is generally performed:
How the Test is Performed
- Nerve Location: The practitioner identifies the median nerve that passes through the carpal tunnel in the wrist. The carpal tunnel is located on the palmar aspect of the wrist, and the median nerve is one of the components of this tunnel.
- Light Tapping: The professional performs a light tapping on the skin directly above the median nerve, usually on the volar side (palm side of the hand).
Interpretation of the Test
- Positive: A positive result is indicated if the patient feels tingling, tingling, or electrical sensations along the path of the median nerve during tapping. This may suggest irritation or compression of the median nerve at the carpal tunnel.
- Negative: The absence of abnormal sensations during tapping is considered a negative result.
Phalen test
The Phalen test, also called the wrist flexion test, is a diagnostic test used to evaluate the presence of carpal tunnel syndrome, a condition where the median nerve is compressed at the wrist. This test is named after Dr. George Phalen, who first described it.
How the Test is Performed
- Basic Position: The patient is asked to hold the wrists in maximum flexion, elbows extended, palms facing each other and fingers pointing down.
- Position Hold: The patient maintains this position for one minute or until symptoms such as tingling, numbness, or pain appear.
Interpretation of the Test
- Positive: The presence of symptoms (tingling, numbness, pain) in the first three fingers and half of the fourth finger within 1 to 1.5 minutes is considered a positive result. This suggests possible compression of the median nerve at the level of the carpal tunnel.
- Negative: The absence of symptoms for the duration of the test is considered a negative result.
Managing Carpal Tunnel Syndrome: What to Do and When to Seek Help
Management of carpal tunnel syndrome (CTS) may involve different approaches, depending on the severity of symptoms and response to treatments. Here are some general recommendations for managing carpal tunnel syndrome:
- Medical Consultation: If you experience symptoms such as numbness, tingling, pain or weakness in the hand and wrist, consult a healthcare professional, usually a general practitioner or orthopedist. An accurate diagnosis is essential to determine the best treatment approach.
- Splints: For mild to moderate cases, wearing wrist splints, especially at night, can help keep the wrist in a neutral position, reducing pressure on the median nerve. Splints may be recommended by your doctor.
- Activity Modifications: Avoid repetitive wrist movements which can worsen symptoms. Ergonomic adjustments at work or at home can also be helpful.
- Exercises: Certain specific exercises, under the supervision of a healthcare professional, can help strengthen the wrist muscles and improve stability. Physical therapy may be recommended.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to relieve pain and inflammation. Diuretic medications may also be considered in some cases to reduce swelling.
- Corticosteroid Injections: In cases where pain is persistent, corticosteroid injections directly into the carpal tunnel may be recommended to reduce inflammation.
- Surgery: If symptoms do not improve with conservative treatments, surgery may be considered. Carpal tunnel release is a common and effective procedure to relieve pressure on the median nerve.
- Weight Management: Maintaining a healthy body weight can help reduce pressure on joints and nerves, which can be particularly beneficial in CTS.
- Avoiding Occupational Risk Factors: If your job involves repetitive wrist movements, regular breaks and ergonomic adjustments may be recommended to prevent CTS from getting worse.
- Regular Medical Follow-up: If you have undergone surgery or are following conservative treatment, regular medical follow-up is important to assess progress and adjust the treatment plan if necessary.
Why Wearing a Wrist Splint Can Help Relieve Carpal Tunnel Symptoms
Wearing a splint for carpal tunnel syndrome can be an important part of conservative treatment aimed at relieving symptoms and reducing pressure on the median nerve. Here is some information about wearing a splint for carpal tunnel syndrome:
- Purpose of the Splint: The splint is designed to keep the wrist in a neutral position, that is, neither too bent nor too extended. This helps reduce pressure on the carpal tunnel, relieving symptoms such as numbness, tingling and pain associated with CTS.
- Timing of Wear: The splint is often recommended to be worn at night while sleeping. CTS symptoms tend to be more pronounced at night, and wearing a splint can help prevent wrist positions that could worsen symptoms during sleep.
- Occasional Daytime Wear: In some cases, your healthcare professional may recommend occasional wear of the splint during the day, especially during activities that could trigger symptoms, such as prolonged typing on a computer keyboard.
- Comfort and Fit: It is essential that the brace fits correctly to provide effective support. It should be comfortable to wear, but snug enough to keep the wrist in the desired neutral position.
- Medical Follow-up: Wearing the splint is generally part of a larger treatment plan. Your healthcare professional can give you specific advice on how long you should wear the splint and how to incorporate its use into your daily routine.
- Alternatives: In addition to traditional braces, there are specific braces designed to be worn during specific activities, such as typing on a computer keyboard. Your healthcare professional can advise you on the type of splint best suited to your needs.
- Combination with Other Treatments: Splinting is often combined with other conservative treatment approaches, such as physical therapy, specific exercises.

- Wear a day splint to limit movement

Osteopathy for Carpal Tunnel Syndrome: Gentle Techniques for Relief
- Approach for carpal tunnel syndrome:
- Osteopathy may include techniques to improve wrist mobility, release muscle tension and promote better blood circulation. Gentle mobilizations can be used to reduce restrictions in the soft tissues surrounding the carpal tunnel.
- Treatment of the cervical spine:
- For people with double crush syndrome, where there is compression in both the cervical spine and the wrist, the osteopath may focus on treating the cervical region. This may include gentle mobilizations aimed at improving the mobility of the cervical vertebrae, reducing muscle tension and promoting nerve circulation.
- Myofascial release technique :
- The practitioner places his fourth and fifth fingers of both hands between the patient’s fourth and fifth fingers and the first and second fingers of the palmar surface (Figure 9A). The patient’s wrist is placed in dorsiflexion and the practitioner’s thumbs cover the lateral and medial attachments of the wrist flexor retinaculum (transverse carpal ligament) (Figure 9B). Transverse distraction is applied to the retinaculum using a 3- or 4-point flexion technique, with 2 ventral points and 1 to 2 dorsal points until soft tissue relaxation or release of restriction is achieved (Figure 9C ). In cases where dorsiflexion causes CTS symptoms, myofascial release can be performed without dorsiflexion of the wrist.
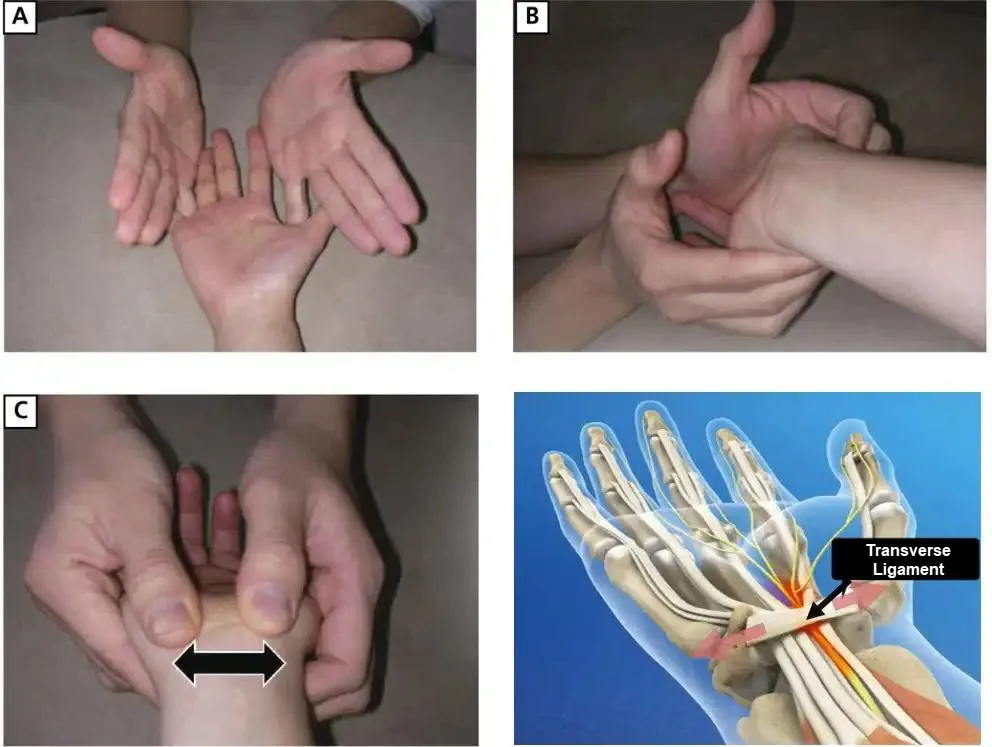
Sucher’s study presents strong evidence for the therapeutic value of osteopathic manipulation for the treatment of carpal tunnel syndrome
- Dr. Sucher developed a comprehensive model for the clinical, electrophysiological, and graphical assessment of carpal tunnel syndrome (CTS). In his work, he demonstrated pathological changes perceptible during neurological examination, using latency studies of the distal nerve as well as magnetic resonance images of the carpal tunnel to measure its volume 1 .
- Subsequently, Dr. Sucher began treating his patients using specific osteopathic manipulations. The results of its interventions have been evaluated in depth. He noted a clear objective improvement in neurological outcomes, distal nerve latencies and carpal tunnel volume, measured by magnetic resonance examinations 1 .
- These observations suggest that osteopathic manipulations may play a beneficial role in the management of carpal tunnel syndrome. However, it is important to note that additional research and clinical studies are needed to confirm these results and establish the effectiveness and safety of this approach in the treatment of CTS.
Stretching and Strengthening: Exercises to Relieve Carpal Tunnel Symptoms
- Median nerve stretch:
- Place your affected hand in prayer position in front of your chest, with fingers pointing upward.
- Slowly lower your hand downward, keeping your fingers in prayer position.
- You should feel a stretch along your arm and wrist. Hold the position for 15 to 30 seconds and repeat several times.
- Slipping of the tendons:
- Hold your hand in front of you with fingers pointing down.
- Use the other hand to gently bend the fingers upward, stretching the tendons.
- Hold the position for a few seconds, then slowly release. Repeat several times.
- Tendon gutter exercise:
- Place your forearms on a flat surface, with your wrists and hands hanging over the edge.
- Gently flex your wrists, raising and lowering your fingers.
- Repeat this movement several times, making sure to maintain a gentle movement.
- Stress ball exercise:
- Hold a stress ball in the affected hand.
- Squeeze and release the stress ball repeatedly to strengthen hand muscles and improve circulation.
- Forearm stretch:
- Extend the affected arm in front of you, palm facing down.
- Use the other hand to gently pull the fingers back until you feel a stretch on the upper side of the forearm.
Frequently Asked Questions About Carpal Tunnel Syndrome
- What is carpal tunnel syndrome (CTS)? Carpal tunnel syndrome is a medical condition characterized by compression of the median nerve at the wrist, leading to symptoms such as numbness, tingling, muscle weakness, and sometimes pain in the hand and arm.
- What causes CTS? Causes of CTS may include inflammation, trauma, repetitive activities, predisposing anatomy, underlying medical conditions, and other factors. Certain groups, such as pregnant or postmenopausal women, are more likely to develop this condition.
- How is CTS diagnosed? CTS can be diagnosed by clinical tests such as Tinel’s sign and Phalen’s test. Additional tests, such as electromyography (EMG) and nerve conduction, may also be used to confirm the diagnosis.
- What are the symptoms of CTS? Symptoms of CTS include numbness, tingling, muscle weakness, pain radiating from the wrist down the arm, and nighttime sensations. These symptoms may worsen at night.
- What treatments are available for CTS? Treatment for CTS depends on the severity of the symptoms. It may include conservative measures such as wearing splints, anti-inflammatory medications, osteopathy, and in some cases, surgery.
- Are there any risk factors associated with CTS? Yes, several risk factors are associated with CTS, such as repetitive work, wrist position, gender (more common in women), age, pregnancy, obesity, and some specific medical conditions.
- Can the CSC be notified? Some preventive measures include practicing exercises and stretching, taking frequent breaks from repetitive activities, ergonomic adjustments, and managing risk factors.
- What is the difference between CTS and “double crush syndrome”? “Double crush syndrome” is a controversial concept. Although CTS is associated with nerve compression at the wrist, the idea of double compression, also involving the spine, is the subject of debate within the medical community.
- Are osteopathic manipulations recommended for CTS? One study mentioned suggests that osteopathic manipulations may have beneficial effects in the management of CTS, but this remains subject to debate and requires individual assessment by a healthcare professional.
- When should I see a healthcare professional for CTS-related symptoms? If you experience persistent symptoms such as numbness, tingling, or pain in your hand and arm, it is recommended to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Carpal Tunnel Knowledge Check: Advanced CTS Quiz
1. Which nerve is most commonly compressed in carpal tunnel syndrome?
- A) Ulnar nerve
- B) Radial nerve
- C) Median nerve
- D) Ulnar nerve
- E) Fibular nerve
2. What is the main difference between CTS and tenosynovitis?
- A) CTS affects the knees, while tenosynovitis affects the wrists
- B) CTS is inflammation of the joints, while tenosynovitis is inflammation of the tendons
- C) CTS is mainly caused by infections, while tenosynovitis is linked to muscle damage
- D) CTS is a chronic condition, while tenosynovitis is acute
- E) CTS affects adults, while tenosynovitis affects children
3. What is the commonly used surgical treatment for CTS?
- A) Arthroscopy
- B) Osteotomy
- C) Carpal tunnel release surgery
- D) Blood transfusion
- E) Skin graft
4. What work activity is often associated with an increased risk of CTS?
- A) Office work
- B) Construction
- C) Fishing
- D) Professional musician
- E) No known professional correlation
5. What is the potential untreated complication of CTS?
- A) Heart failure
- B) Muscle atrophy
- C) Blindness
- D) Urinary incontinence
- E) Ossification of the joints
Answers
- C) Median nerve
- B) CTS is inflammation of the joints, while tenosynovitis is inflammation of the tendons
- C) Carpal tunnel release surgery
- B) Construction
- B) Muscle atrophy
Final Thoughts: Better Understanding for Better Treatment of Carpal Tunnel Syndrome
Carpal Tunnel Syndrome (CTS) is a medical condition resulting from the compression of the median nerve at the wrist. This compression can be caused by various factors such as inflammation, trauma, underlying medical conditions, predisposing anatomy, repetitive activities, and other factors. Symptoms include numbness, tingling, muscle weakness, pain radiating from the wrist down the arm, and nighttime sensations.
CTS is more common in women, especially during pregnancy and menopause. Diagnostic tests such as Tinel’s sign and Phalen’s test can assess the presence of CTS. Treatment varies depending on the severity of symptoms and may include conservative measures such as splints, anti-inflammatory medications, osteopathy, and, in some cases, surgery.
There is controversy surrounding the concept of double crush syndrome, emphasizing that the understanding of nerve pathology has evolved since its introduction. The osteopathic approach is discussed, citing a study by Dr. Sucher, suggesting that osteopathic manipulations may have beneficial effects in managing CTS.
Risk factors such as repetitive work, wrist position, gender, age, pregnancy, obesity, and specific medical conditions may contribute to the development of CTS. Recommendations include exercises and stretches, changes in daily activities, specific therapies, and symptomatic treatment approaches.
It is essential to emphasize that anyone experiencing persistent symptoms should consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
References
- American Academy of Orthopedic Surgeons. (nd). Carpal Tunnel Syndrome. https://orthoinfo.aaos.org/en/diseases–conditions/carpal-tunnel-syndrome/
- Szabo, R. M. (1989). Carpal Tunnel Syndrome as a Repetitive Motion Disorder. Clinical Orthopedics and Related Research, 243, 78–89.
- Atroshi, I., Gummesson, C., Johnsson, R., Ornstein, E., & Ranstam, J. (1999). Carpal tunnel syndrome in the general population: Prevalence and risk factors. Journal of the American Medical Association, 282(2), 153–158. https://doi.org/10.1001/jama.282.2.153
- Wilson J 0, and a1. Harrison’s Principles of Internal Medicine, 12th ed. New York, NY: McGraw-Hill; 1991: 1487
- Armstrong T.J. An Ergonomics Guide to Carpal Timnel Syndrome. Ergonomics Guide Series. Akron, OH: American Industrial Hygiene Association; 1983.
- H il tz R. Fighting work-related injuries. Underwriter Nation. 1985;89:15.
- Upton A, McComas AJ. The double crush in nerve entrapment syndromes. Lancet. 1973;2:359.
- Abramson 01, Rickert BL, Alexis JT, et al. Effects of repeated periods of ischemia on moror nerve conduction. J App! Physiol. 1 97 1;30:636-642.
- Larson NJ. Osteopathic manipulation for syndromes of the brachial plexus. J Am Osteopath Assoc. 1972;72:94-100.
- Hurst LC, et al. The relationship of double crush syndrome ro carpal tunnel syndrome (an analysis of I,000 cases of carpal tunnel syndrome). J Hand SlIrg. 1985; 10:202.
- Sunderland S. The nerve lesion in the carpal runnel syndrome. J Neurol
Neurosurg Psychiatry. 1976;39:615. - Sucher BM. Palpatory diagnosis and manipulative management of carpal tunnel syndrome . Am Osteopath Assoc. 1994;94:647-663.
- Sucher BM. Myofascial manipulative release of carpal tunnel syndrome : Documentation with MRl. Am Osteopath Assoc. 1993;93:1273-1278.